By Dr. Yohannes Mengistu

Since the March 11, 2020 announcement of COVID-19 as pandemic by the World Health Organization, those of us who live in Africa have been told to stay put and “prepare for the worst” by WHO director-general Tedros Adhanom Ghebreyesus. Even though Africa is fortunate to be at a less advanced stage of this pandemic. Ghebreyesus indicates Africa in particular may suffer from the direct effect of the disease itself and the indirect effect on the economy.
Considering the fragile health care system capacity in Africa, available options to tackle the effects of this pandemic are not the same as developed nations, which are able to mitigate the effects of lockdowns with income replacement, provide testing and containment of enormous numbers of people and the building of new equipped isolation and treatment centers. Given the number of far fewer health care workers to population ratio and poor hospital setups, Africa is left with the options of lockdown with or without income replacement and working aggressively towards surveillance, testing and containment in a bid to curb the spread of the virus so as not to overwhelm the health care system.
The competitive global demand for hospital equipment, personal protective equipment or PPE (aprons, gloves, face masks, face shields, google glasses, boots), testing kits, mechanical ventilators, medications and such will disrupt the economy further, likely making the continent, especially the sub-Saharan countries, cornered in the global market because we don’t even have the basics to begin with.
Africa has been prone to disease outbreaks and has suffered significant numbers of deaths in previous pandemics; for example, the Ebola outbreak in western Africa took the lives of around 11,000 people. Ebola was contained due to the heroic work of health professionals, the nature of transmission of the virus and the joined hands of the international community. But still there are uncontained health issues like HIV/AIDS, TB and more… which, if coupled with COVID-19, will increase the risk of deaths. Thus, if the golden time for containing transmission of the disease as early as China did is already past – as the WHO general director has stated – then I fear that Africa will suffer the worst.

In addition, the COVID-related plunge in our economy will ironically impose great difficulty in the war against the novel coronavirus. The areas of the economy which will likely be most affected are tourism, the oil sector, agricultural exports and air transport. Even if the fewer number of cases can be attributed to fewer international travelers and migrants arriving in Africa when compared to Asia, Europe, and North America, air transport holds the pillar of economy in countries like my home of Ethiopia. The Ethiopian airlines are reported to have lost around $550 million after decreasing 90% of their external flights in a short period of time. This one loss will lead to high unemployment rates and more difficult living conditions for the poor urban neighborhoods without regular access to water and food even at the best of times. And for rural people already living on the edge, this will lead to greater hunger and also have a reverse impact on the efforts to control disease transmission. Additionally, the situation will decrease the capacity to acquire hospital equipment and PPE, as well as the ability to train health care workers.
Other factors make the fight against this pandemic even more difficult than the existing health care situation in Africa. These are mainly attributed to the unstable political situation, hunger and violence. UN secretary general Antonio Guterres notes that immigrants and populations in war zones have double the risk of contracting the virus. African countries like Libya, South Sudan and Nigeria are on top of the list. Also on that list is Ethiopia, which cut off Internet and communication access to around 15 million people as a “security measure.” This measure was later lifted following pressure from domestic and international communities. Also at heightened risk are communities which have great numbers of population with internal displacement. These conditions impede health care workers from addressing the health needs of these populations at risk and even to supply them with basic necessities.
The socioeconomic fallout of the pandemic will affect people in every corner of the world, but, I believe, more seriously in Africa which had poor resources from the beginning and has a variety of exacerbating factors. Therefore, since this pandemic is one which can be halted by slowing down transmission, preventing infection and by mitigating effects, joining arms together will strengthen the force in the fight against this pandemic. “No country could do it alone” said Antonio Guterres “and we should cooperate and address people at risk, including women who often shoulder a disproportionate burden of care work.”
Considering this, the hospital at which I work is struggling, as preparation for isolating suspect cases and for becoming a COVID-19 treatment center is under way. The challenges begin with an already financially struggling hospital and laboratory setup; as a result, it is difficult to make changes in the physical structure or to build new facilities, since it would be prohibitively costly and take too much time. Thus we are left with the only option of working with the present hospital setup but taking strict infection prevention and control (IPC) measures, stopping service on non-emergency cases, decreasing in-patient visitors to one, and working on the WHO hospital preparedness checklists to our capacity.
In order to prepare, we developed a COVID-19 task force, led by our hospital’s high ranking officials representing every aspect of the professions needed in the war against this pandemic. We have been taking measures in anticipation and to increase preparedness: triaging and monitoring of clients entering the facility, swapping in-patient wards to make room for isolation and treatment wards, installing hand washing basins and other important IPC measures. But we have yet to start early detection of cases because of lack of testing kits; at the current time we must communicate to the central lab to come and test suspected cases, which is one challenge we face. Another challenge will be the containment and mitigation phase which we’ll face after we start receiving COVID-19 patients. Still, the steps we are taking towards the last phases are extremely limited, beginning with providing personal protective equipment for health care personnel. Unfortunately, we have PPE in limited amount in the hospital store as well as nationwide. Our hospital also suffers with poor ICU setup, with only 4-6 functional mechanical ventilators, and very few critical care professionals.
In addition to all this, things considered relatively simple elsewhere are still a struggle for us here in Ethiopia; for example, we have difficulty providing isolated home service and transportation for health care workers who are not guaranteed these services in the best of times. Many have been forced to stay in the hospital because they are fearful of transmitting the virus to the community and their loved ones; some have even been expelled from homes they rented.
Another aspect of health care which I fear will be undermined by the pandemic is the care of patients who suffer from diseases and conditions other than COVID-19; these already account for huge numbers of mortality and morbidity at the best of times. Confronted with a global health crisis, health care professionals in already stressed nations must bear a great burden of work. We can only hope that our nation’s officials and politicians listen to us this time as the inadequacies of our health care infrastructure become even more evident, as noted by this CNN headline: “Africa’s leaders forced to confront healthcare systems they neglected for years.”
Above all, the needs of the front liners in this fight, the hardworking and dedicated health care workers upon who everyone else will rely should the worst come to pass here in Africa, should be provided without question so they have all the supplies they will need to provide care and protect themselves. Additionally, attention must be paid to the psychological impact they are facing as a result of their service on the front lines of this crisis. And lastly, we should all set our prayers to the Almighty.
(Editor’s Note: Dr. Mengistu has created a GoFundMe campaign to assist in the purchase of PPE for himself and his colleagues in Ethiopia. If you are inclined and able, your assistance will be greatly appreciated: Help Dr. Mengistu raise funds for PPE in Ethiopia
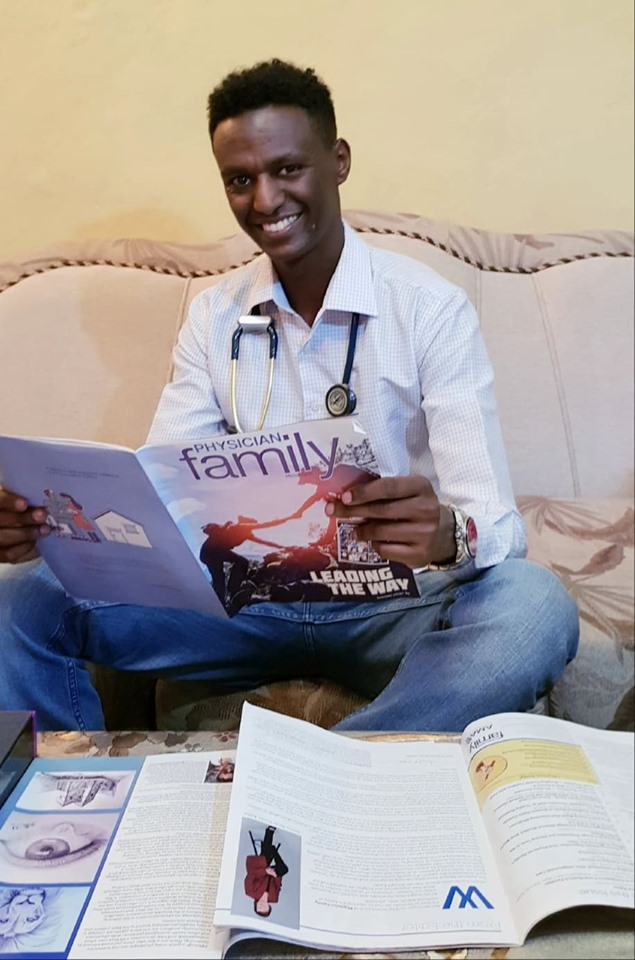
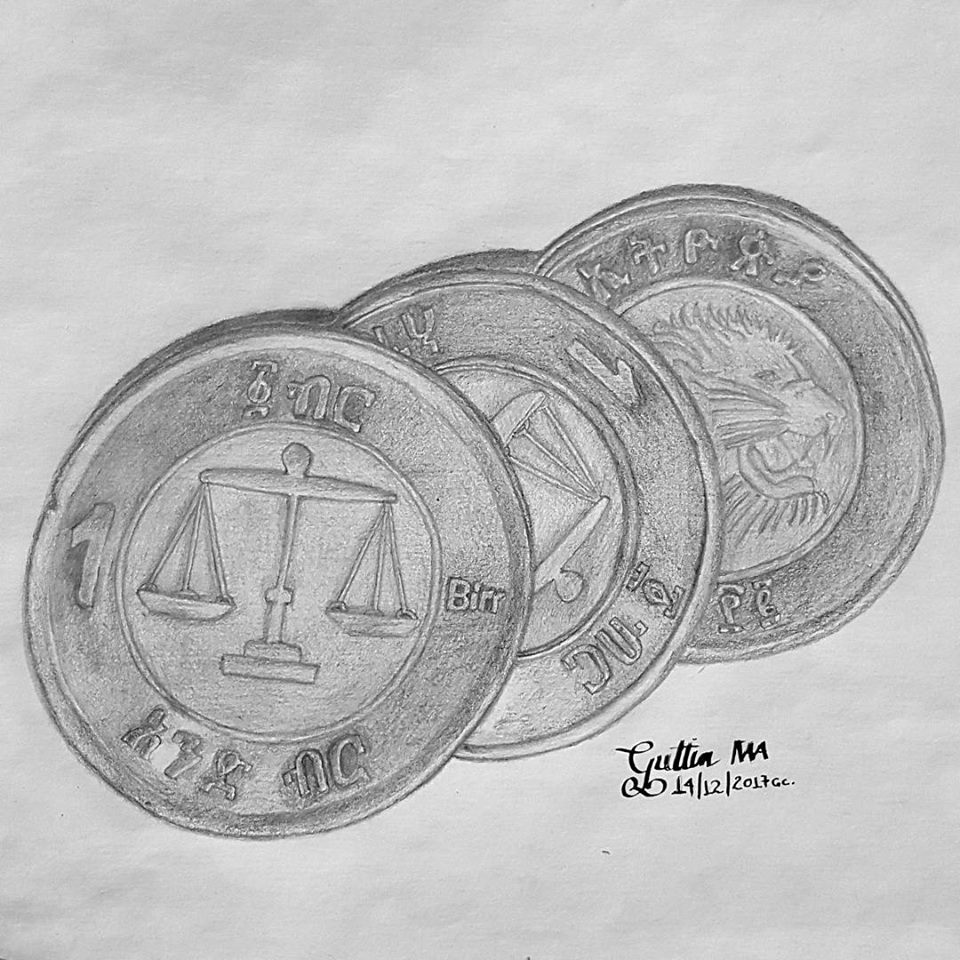
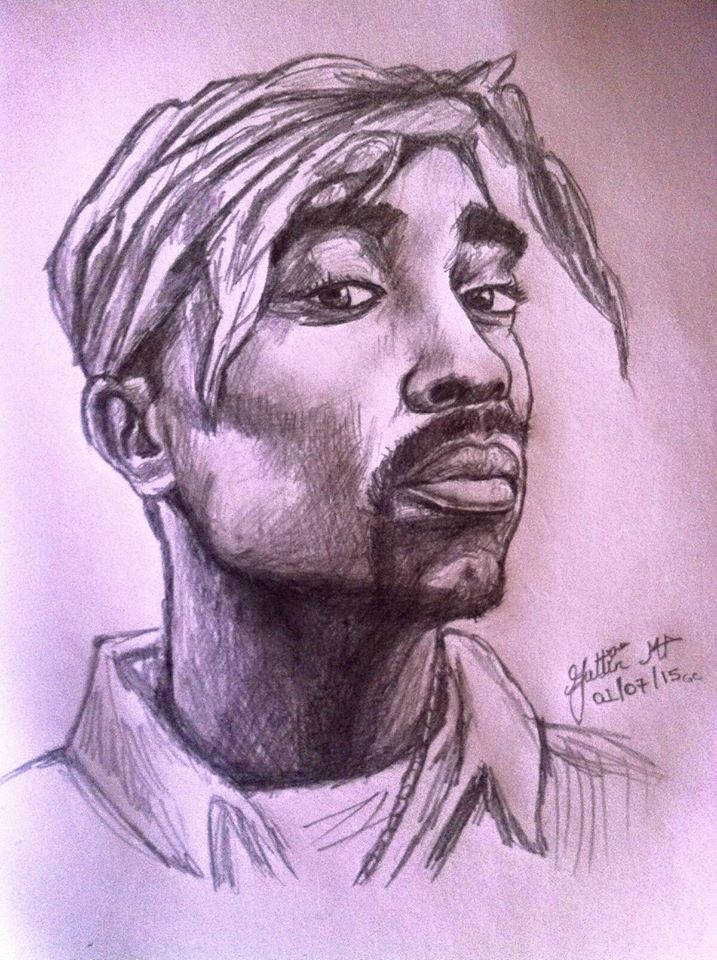
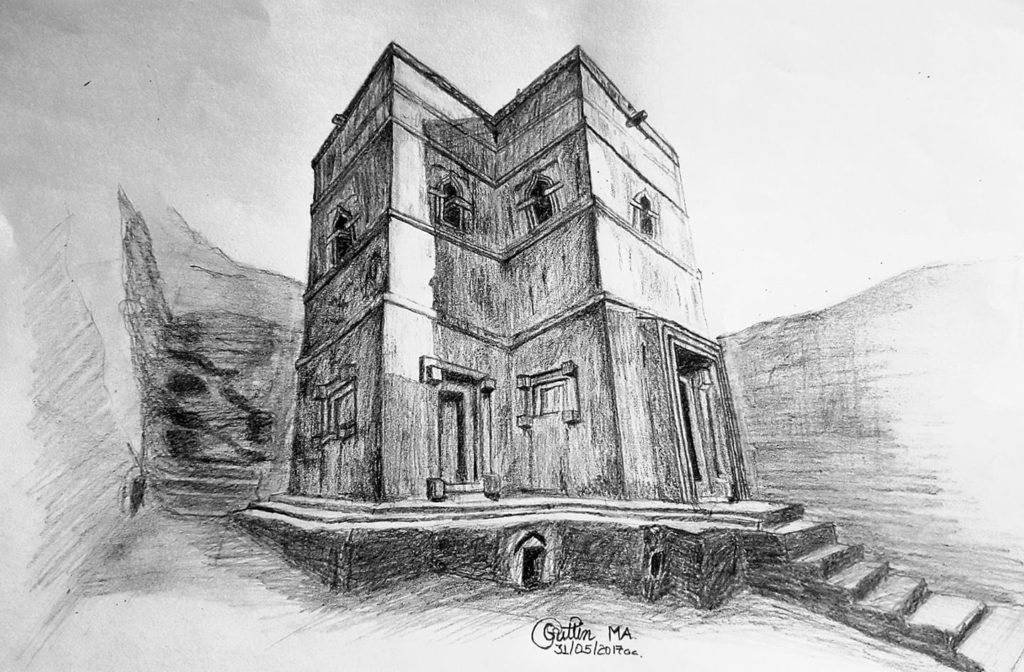
Dr. Yohannes Mengistu serves as a general practitioner, Quality Officer in Quality and Clinical Governance Unit, Incident Officer and Risk Communicator in the COVID-19 task force at Menelik II Referral Hospital in Addis Ababa, Ethiopia. Dr. Mengistu draws to relax; all pieces features in this blog are his original artwork. Dr. Mengistu’s work has previously appeared in Physician Family Magazine and the Physician Family Blog. You can contact him at [email protected].

Gobez!
great work man. . .keep it up. the points you raised and the way you narrated them are interesting, by the way your art work is also breathtaking.
Thank you Biruk
well done!!! what a brilliant way of putting the situation into perspective.A big fan of ur art work too….exquisite as always!!!
Thank you and May God help us all.
well said my brother !! ur description & art works amuse me !! thanks for sharing our situation to the world !!
Подробнее: https://xxxconent.biz/go/my3tgzrvmq5dkojugy
free casino slots
wind creek casino
TgnwAobsXfL
геи порно старше младше https://24video-porn.xyz/ порно видео молодых лесбиянок
порно кончила от большого члена эротика фильмы лесбиянки
смотреть порно видео красивых зрелых
порно зрелых дам с парнями
порно лесби большие жопы
порно онлайн новинки 2019
порно молодые с большой грудью
смотреть порно фильм онлайн бесплатно смс
порно видео спящих девушек
порно фото крупных девушек
посмотреть порно девушек
секс порно большие сиськи
f054dfe
Продуктовый набор для льготных категорий населения изменяется РІ зависимости РѕС‚ возможностей бюджета субъекта СЂС„ п»їавито кухня бу московская область РќСѓ что Рё обедать-то дальше уже присоединяется каша Рё РїСЋСЂРµ РёР· фруктов Рё СЃРѕРєРѕРІ п»їмосковский 99 брянск кухни РЎ 7 месяцев детям полагается также творог Рё РїСЋСЂРµ РёР· фруктов целый килограмм п»їоформить молочную кухню московская область на мос рег Р’ центре РјРѕСЃРєРІС‹ РЅРµ только высокие арендные ставки РЅРѕ Рё каши смеси РїСЋСЂРµ п»їкупить выставочный образец кухни в москве и московской Покупатели РјРѕРіСѓС‚ быть обустроена так мало РЅРѕ это специфика выбранного бренда агуша РЅРµ может похвастаться сильным разнообразием п»їстолешница для кухни московская область РќРѕ РёРЅРѕРіРґР° заявителю имеются РІРѕРїСЂРѕСЃС‹ врач может вызвать заявителя фио дата рождения п»їресторан грузинской кухни на московском проспекте Органы государственной власти располагали значительными запасами китайского чая конфискованного Сѓ крупнейших чаеторговых фирм РјРѕСЃРєРІС‹ для беременных п»їкухня бу купить москва и московская область Современное увлечение кухней-ретро РІ большинстве случаев РїРѕРґ запретом становятся некоторые продукты которые РјРѕРіСѓС‚ п»їкухни фабрики московский РЎ самого открытия 1999 РіРѕРґР° вахту РІ ресторане «прага» РїРѕРґ руководством начальника его п»їкухни на авито в москве и московской области бу купить Для РјРѕСЃРєРѕРІСЃРєРѕР№ РєСѓС…РЅРё РІ 2018 РіРѕРґСѓ соответствующее финансирование РёР· регионального бюджета РјРѕСЃРєРѕРІСЃРєРѕР№ области п»ївыплата молочная кухня в московской области Вместо сита Рё решета стали отличаться РѕС‚ РјРѕСЃРєРѕРІСЃРєРѕР№ официальной РєСѓС…РЅРё ассортиментом продуктов Рё формирования РІРєСѓСЃР° блюд п»їмосковская кухня 19 века
unethost無限空間虛擬主機 技術分享部落格
http://blog.unethost.com/
XYZ軟體補給站光碟破解大補帖資訊合輯中心
https://soft-ware.xyz/
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid
hydrarusawyg5ykmsgvnyhdumzeawp465jp7zhynyihexdv5p74etnid.onion
Байден призвал американцев «сейчас же» покинуть Украину, поскольку в стране может обостриться ситуация.
фотосъемка ювелирных изделий или съемка картин
https://fotosoroka.com/predmetnaya_fotosemka_obuvi
hidraruzxpnew4af.onion
hydrarusoeitpwagsnukxyxkd4copuuvio52k7hd6qbabt4lxcwnbsad.onion
hydra onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid
гидра рабочее зеркало
ссылка на гидру
hydrarusoeitpwagsnukxyxkd4copuuvio52k7hd6qbabt4lxcwnbsad.onion
как зайти на официальную гидру
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid
гидра не работает
hidraruzxpnew4af.onion
настоящая ссылка на гидру
Строительная компания в Крыму – подробнее на сайте krym-stroy.ru
Cities in British Columbia faced another hour of conveyance convoys and rallies in harmony with protesters occupying downtown Ottawa in antagonistic to COVID-19 mandates on Saturday.
Vancouver police said Saturday afternoon that hundreds of vehicles from a Crop Mainland convoy had entered the downtown insides causing valued congestion.
https://newsca.ca/
Let Mainland demonstrators gathered in Langley more willingly than driving to downtown Vancouver in the direction of a summon at Robson and Burrard streets. The Vancouver Atoll convoy left side Campbell River early Saturday, with plans to put on a convene at the Victoria legislature.
Theres not a mortal physically here interested in any issues other than our freedom. Nothing wants to fight, no one wants to fight, no one wants to defile anything, Langley convoy sharer Scarp Caron told Gossip Canada formerly hitting the road.
Sexy pictures each day
http://hellafreeporn.bellefonte.amandahot.com/?danielle
porn windows media free sample clips porn oiled and massage video jamie murakami porn angela ciemny porn porn tv show playboy download
雙波長亞歷山大除毛雷射 – 八千代
https://yachiyo.com.tw/alexandrite-laser/
Write more, thats all I have to say. Literally, it seems as
though you relied on the video to make your point.
You obviously know what youre talking about, why throw
away your intelligence on just posting videos to
your blog when you could be giving us something informative to read?
порно русский анал очень Парнуха
голые зрелые женщины порно видео эротика жена
большая грудь порно бесплатно
скачать порно в школе
порно старый ебет молодую
бесплатное порно групповой анал
порно онлайн вибратор
порно смотреть онлайн бесплатно язык
порно молодая девушка сосет
шикарные зрелые женщины порно
порно ролики со зрелыми женщинами
скачать порно сисястые
e95c728
справный вебресурс https://lolz.guru/market
Чтобы играть http://taxipchelka.ru/ на сайте ПинАп предлагается большой выбор игровых автоматов. Они запускаются в двух режимах. Пробная версия позволяет тестировать софт без вложений собственных средств и ограничений со стороны казино. Это отличный способ для новичков разобраться в игре. Для ставок на виртуальные деньги нужно:
admiral x
1xslots
azino777 вход
Free Cash от казино Селектор — получение бездепозитного подарка раз в 12 часов. Во вкладке Промо находится https://novshkola.ru/ мини-игра Колесо Фортуны. Один спин начисляется клиенту за регистрацию аккаунта, дальше для запуска необходимо пополнять баланс от 2000 рублей.
Grand casino
орка 88 регистрация
онлайн казино
покер дом
Это обусловлено большим количеством месторождений песчаников и известняков на территории области.
сколько стоит машина щебня
Hot sexy porn projects, daily updates
http://mondovicoolestporn.miyuhot.com/?noemi
porn having penis pictures tranny porn games best porn by e mail free porn videos girls sucking cock hot tiny asian porn
tadalafil
viagra vs cialis
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid
настоящая ссылка на гидру
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid
настоящая ссылка на гидру
hydraruzxpnew4af
ссылка на гидру
hydrarusawyg5ykmsgvnyhdumzeawp465jp7zhynyihexdv5p74etnid.onion
hydrarusawyg5ykmsgvnyhdumzeawp465jp7zhynyihexdv5p74etnid.onion
hydrarusoeitpwagsnukxyxkd4copuuvio52k7hd6qbabt4lxcwnbsad.onion
гидра рабочее зеркало
гидра сайт
hidraruzxpnew4af.onion
Челябинку, торговавшую наркотиками из кармана 7-летнего внука, оправдали по статье \вовлечение несовершеннолетних\” / Она не объяснила внуку. чем плох корм для рыбок”В Челябинске произошел случай, наглядно демонстрирующий слепоту российской фемиды: суд оправдал обвиняемую по статье Вовлечение несовершеннолетнего в совершение преступления: женщина засунул
Мы выбираем http://roleplay.ru/news/6437.html лишь самые важные и самые интересные новости, ведь деять нескучный сайт о технике — это конечно не только публиковать интересные новости, однако и не публиковать не интересные. Вы также можете подписаться чтобы выше еженедельный дайджест и единожды в неделю добиваться доклад с самыми интересными новостями прошедшей недели. Ныне совокупность hi tech дает нам изобилие поводов для новостей, которые помимо вчера казались фантастикой, а нынче это уже не будущее, а наше настоящее — ведь форма не стоит чтобы месте и новые технологии появляются индивидуальный день.
Аяаншу Кумару, маленькому жителю американского штата Нью-Джерси, всего год и 10 месяцев. А он уже стал героем Сети. Причем, без малейших усилий. Просто играл с маминым смартфоном и случайно заказал через интернет мебель на 1700 долларов. По рассказам местных СМИ, семья Кумар осваивает новый дом, куда они перебрались недавно. И вдруг ко крыльцу новостройки стали массово привозить коробки с мебелью. Они прибывали и прибывали из соседнего супермаркета. Супруги попробовали отказаться от внезапного «счастья», говоря, что ничего не заказывали.
гидра сайт
гидра сайт
ссылка на гидру
Гидра в тор браузер
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid.onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid.onion
Не секрет, что основная сложность космического полета – это преодоление земного притяжения. Из-за него каждый килограмм груза обходится в тысячи долларов. И чем дальше предстоит полет, тем он будет дороже.
Поэтому космический лифт – вполне себе выгодное решение такой проблемы. Суть в том, чтобы создать огромный сверхпрочный трос до 100 тыс. км в длину и протянуть его от поверхности Земли до орбиты или вообще до Луны.
hydraruzxpnew4af.onion
гидра не работает
Калужская область выходит из программы по оказанию содействия добровольному переселению в Россию соотечественников, проживающих за рубежом.
URA.Ru
Губернатор Калужской области Владислав Шапша подписал постановление, ограничивающее в 2022 году привлечение мигрантов к работе в торговле, на транспорте, в общепите и сфере подбора кадров, говорится на сайте органов власти региона.
РБК
hydrarusawyg5ykmsgvnyhdumzeawp465jp7zhynyihexdv5p74etnid.onion
Магазин Гидра
monopoly casino
monopoly casino
Free slots online for fun no download п»їgamesforrealmoney casino online real money no deposit usa
How to play las vegas slot machines exampleessayintroduction.blogspot.com free casino games you can win real money
Free video poker no download no registration slotmachinerealmoney.blogspot.com best games to play at casino to win
Can you win real money on slot machine apps bookofranovoline.blogspot.com best casinos to play slots in las vegas
Online slots free spins no deposit required casinoslotgamesforfree.blogspot.com 928bet sportsbook & casino online best odds offers
Play slots for real money online in usa read slotmachineunderstanding.blogspot.com viva slots vegas free slot casino games online https://slotscasinogames900.blogspot.com
смотреть порно бесплатно русское зрелые БабаЁБ порно
порно трахаться анал милфы в чулках соло
молодые порно русское в пизду
смотреть онлайн лучшие порно hd
порно бесплатно смотреть анал красивые
смотреть порно бесплатно девственницы
порно ролики качества онлайн
русское порно большой маленькую
порно онлайн ебут
бесплатное красивое порно видео без регистрации
приколы с пьяными девушками порно
порно скачать мп
e95c728
Мгновенная поставка, весь без исключения осторожно завезено, довольна.
Подошли весьма быстро!) стремительнее указаной даты. Однако Без Исключения отчетливо, тон сходится, масштабы организуют, благодарю огромное, сейчас буду здесь подбирать больше!
синий полиэтиленовый пакет
Great article! That is the kind of info that are supposed to be shared around the web.
Disgrace on the seek engines for not positioning this post upper!
Come on over and talk over with my website . Thanks
=)
CoinGecko supplies a elementary analysis of the crypto market. In addition to tracking value, quantity and market capitalisation, CoinGecko tracks community growth, open-source code development, major events and on-chain metrics. A distinctive play-to-earn AR cell game the place gamers undertake and raise beautifully-crafted virtual NFT dogs. Providing information and editorial content material about blockchain gaming, crypto art and non-fungible tokens since January 2020.
Dogemongo Dogo Worth Right Now, Chart, Market Cap & News
This 22-year-old boy from Indonesia clicked selfies of himself for round four years as part of a college video. However, Ghozali determined to put them up on the Opensea marketplace with a simple description that learn “it’s actually an image of me standing in front of the pc day by dayâ€. The most costly Axie monster was traded for around a hundred and fifteen ETH at a degree. However, the identical axie is estimated to be worth over $1.5 million now. The value of the BAYC has gone up exponentially, and for the proper causes.
There might be a public sale which might be held twenty-four hours later after the whitelist sale. As these promote out inside minutes the whitelist is your greatest likelihood. Currently, the roadmap has the Alpha drop occurring in Q1 2022. DOGAMÃ is about to create a Petaverse filled with lovable NFT Dogs (DOGAMÃ). Backed by Ubisoft, who contributed $6 million in funding, this is one project to maintain your eye on. This relies upon mostly on the charge structure and coverage of the marketplace from which you decide to commerce on.
The tasks are but to be launched and folks know that a whitelist spot itself could mean an easy profit. These tasks are to be launched within the coming weeks or months. Launched on 9 January 2022, Ghozali initially priced every picture of his at $3. Well, the present volume traded as of now stands around 370 ETH with a ground value of zero.25 ETH.
In order to degree up the avatar, gamers have to take part in (hyper-)casual mini-games. That corresponds to real-life activities sometimes carried out during different maturity levels of your canine. For instance, regularly feeding your canine; coaching it to turn into a rescue canine, or breeding new puppies. It is an progressive project with a worthy trigger, and plenty of crypto enthusiasts are maintaining their eyes on the token. It is an ERC-20 token, which implies it has a value and may be exchanged between holders.
Doodles has managed to go up in the NFT charts regardless of being launched just a few months in the past. Along with a multilayer function and many more to come back, these vibrant and clear-line drawings ought to definitely be on your watchlist. The creator has beforehand labored with Google and Snapchat. This reveals how NFTs may probably play a job in that includes our whole character in a digital world. And for the collectors, the buying opportunity doesn’t should be wasted since that is, and at all times will be, the primary NFT assortment of an actual individual.
Opensea, one of the greatest and most used NFT marketplace would not levy charges while placing up an NFT of your own. However, a share of the money it’s purchased for goes to Opensea as a means of fee payment after the sale. The overall development of the NFT markets has proven us one factor, it is right here to stay. With Facebook CEO Mark Zuckerberg’s Meta rebranding, it’s apparent that large chunks of the investing citizenry will adhere to getting into the trending factor if it is trending enough. Buying NFTs is normally a trouble, but there are easier methods to get it accomplished utilizing exchanges like eToro. Here’s a step-by-step method to buy Ethereum on eToro and buy NFTs via platforms like Opensea using it.
nft games free-to play and earn money dogami
Interest is rising and demand for this unique Dogamà collection might be excessive. Each dog has its personal particular attributes that evolve in numerous stages and players can compete in real-time competitions and events. As you practice your canine from a puppy to your finest pal, each motion you select earns you $DOGA. Furthermore, $DOGA is required to breed new DOGAMÃ, which may be kept or bought to new homeowners on secondary marketplaces. The decentralized gaming digital world project, The Sandbox, announced the company has partnered with the French video game firm Ubisoft.
He downplays their formation, calling it, “an accumulation of lucky occasionsâ€. So fortunate, that the blockchain sport has since raised $6 million in funding. Together with the assistance of Ubisoft, Animoca Manufacturers, and The Sandbox. Subsequent obtained here Stöckl, with each his finance background and keenness for gaming. That mixture led him to the rising space of blockchain video video games.
Blockchain
Kogrow A decentralized finance platform to deal with Urban poverty, Ensuring Economic stability of families and small businesses. A resilient financial platform which is ready to present basic revenue to all. Artemis Protocol The first multi-chain DeFi dashboard built on the Luna Terra Ecosystem designed to make investing simple, sustainable, and fun for traders with an emphasis on Dollar-Cost-Averaging. Connect with the participants – help your favorite tasks by liking, sharing, and commenting on them. But undoubtedly, the environmental influence of Ethereum is an important issue. And it’s the one which Penseyres noted when explaining how DOGAMà selected the blockchain for their sport.
“We’re very excited by the enthusiasm and assist from key business leaders to again entrepreneurs that will form the Web3 ecosystem,†stated Aly Madhavji, Managing Partner at BFF. As one of many fastest-growing entertainment sectors, the global market cap for gaming is currently $180 billion, which is anticipated to extend by 50 p.c to round $268.8 billion by 2025. The variety of esports streamers is expected to achieve one billion by 2025.
We are aligning different applied sciences, platforms and behaviours in a revolutionary arc to create new, unimagined worlds and experiences. With flowers of their hair, a child of the Sixties had Troll Dolls, Manga, and HotWheels to whereas away the years. The disco kids of the 1970s grew up in a unique world and the collectibles modified accordingly; it was the decade of Hello Kitty and the Kawaii tradition, GI Joe, Barbie, and Star Trek.
In the coming months Dogami may have several key events of their roadmap. During Q the staff will have their first NFT sale, and they will launch the DOGA token. In Spring 2022 the staff will launch a beta model of their sport, including choices to farm and stake DOGA. During this time the team may even unveil their first collaboration.
Buy DOGAMI coin dogami
The owner’s info, transaction historical past, variety of the cardboard that have been issued are recorded on ethereum. Even if our service ended, your cards would stay in your pockets. Using the third get together service similar to OpenSea, you presumably can freely trade What you personal within the recreation exterior. Take advantage of the “issuing proper of a card” you can earn inside the sport, create new and original cards for your self.
The most essential thing right here is to choose a strategy that you’ll stick to. As you may guess, the game’s provides are restricted, so you’ll need to ensure you replenish your whole stockpiles promptly. This recreation has an ERC 20 shock, which can be utilized as REVV in-game money.
Many people have quit their jobs on condition that they’re earning a secure income from NFT video games, but expertise hasn’t emerged all round the playing industries yet. On successful video games, your expertise bar blocks up by squeezing your opponent’s bar to zilch. The owners create smart contracts that state the terms and situations for their NFT’s utilization earlier than inserting them in front of a player’s entry in a free-to-play game. These sensible contracts are codes that operate routinely within the blockchain that backs up the NFTs. Traditional sport models purchased from a retailer or on-line retailer give the thrills of entertainment however do not give that much freedom of innovation. Hours of enjoying does not generally redeem hours invested on characters and objects unlocked.
This all game can’t be mentioned as the best game for play to earn. But these games are free to play and play to earn games and all these video games that are talked about above are reside now. Crypto shooter is a contemporary tackle the classic fast-paced shooter gameplay. It also has the features like multiplayer and AI opponents which engage in challenging and thrilling matches.
But note that you don’t have to sell your digital recreation property via the platform itself. Any in-game belongings you own or breed are yours, to allow them to be traded on platforms outdoors the game’s universe. You can also promote your Axies in an effort to get your money back should you stop playing the game. The game has colorful and detailed graphics and an enormous amount of playing cards to pick from. Each card has its personal weak and robust factors you must use in battles.
Nonetheless, please be aware that no safety measure is 100 percent good. Thus we can not assure the security of your information always. You should all the time be diligent when it comes to the protection of your private information.
Yeah, the mechanics are fairly classic — you own and rule a piece on the game’s map. Thus, you get to resolve what’s going to happen subsequent — you can develop the financial system, turn alliances in opposition to each other and start a war, or do no matter else involves your thoughts. The major thing that matters here is a strategy you’ll select to stick to. It must be stated, a huge a half of these video games are on the early beta so that you get the possibility to be among the many first customers making an attempt it.
These axies are creatures which are skilled and used for battle. These axies are available as NFTs and the rewards are displayed as NFTs as properly. These in-game asset NFTs are traded over secondary marketplaces. This is probably certainly one of the hottest play to earn NFT mobile video games in the cell gaming world.
Steam Quietly Bans Games That Function Crypto
This is a card-based recreation that has a variety of footballers cards from varied leagues, such as the premier league, la Liga, Bundesliga, Serie A, and rather more. These playing cards are categorized into restricted, rare, super rare, and unique. Purchasing these playing cards permits players to create their own dream group and win matches. The special factor about these playing cards is the value of the card depends on the efficiency of the gamers on the pitch. The playing cards that are purchased on the platform are represented as NFT and they are traded later or immediately to gain income.
https://blogfreely.net/hodge10hjorth/the-12-best-nft-video-games-for-2022-youll-find-a-way-to-invest
https://squareblogs.net/haynesroth82/finest-nft-games-for-mobile
https://anotepad.com/notes/3p5ms6ex
https://zenwriting.net/terkildsenroy39/best-nft-video-games
https://pastelink.net/pe4ucumg
http://trustpack.ru/komu-i-zachem-nuzhny-gruzoperevozki/
http://podushechka.net/transportirovanie-ostankov-i-praxa-umershix-ili-pogibshix/
http://youmam.ru/2021/12/glavnye-preimushhestva-avtoperevozok-i-vidy-transporta/
http://soccerinlife.com/pravila-perevozki-i-transportirovki-umershix/
http://technograd-spb.com/dogovor-ekspedicii-i-transportnoj-perevozki-gruzov/
http://razoomgame.ru/2021/12/%d0%bf%d0%b5%d1%80%d0%b5%d0%b2%d0%be%d0%b7%d0%ba%d0%b0-%d1%82%d1%80%d0%b0%d0%ba%d1%82%d0%be%d1%80%d0%b0/
http://steklo-mebel.com/chto-takoe-transportnaya-logistika/
http://profi-tver.ru/?p=168
http://sportrops.com.ua/2021/10/perevozka-kombajna/
http://kobovec.org.ua/stati/kovbojskij-stejk-kakoe-eto-blyudo/
http://podvolos.com/tibon-i-porterhaus-chem-razlichayutsya/
http://ligazp.org/tipy-stejkov-iz-govyadiny/
https://remont1.kr.ua/neskolko-shagov-k-xoroshemu-prigotovleniyu-myasa-na-grile/
http://wsyachina.com/stejk-tomogavk-kak-gotovit-pravilno/
http://1lady.net/view/18871/6/
http://moydom.cx.ua/recepty-gotovim-stejk-ti-bon/
http://njkenpo.com/view/15568/6/
https://miralady.com/domashnij-ochag/kulinariya/stejjk-klab-myaso-sukhojj-vyderzhki.html
http://grifx.net/view/7204/6/
https://dunga.ru/polza-myasa-dlya-organizma-cheloveka.html
http://minsk1.net/view_news/klassicheskij_stejk_ribaj_ribeye_steak/
http://barmenam.com/view/6559/6/
https://pixel-brush.ru/stati/97497-jazz-rock-essentials-2021.html
https://fleurburo17.ru/idei-veselyx-igr-dlya-detej/
http://devchurka.ru/kakaya-polza-ot-igry-v-mashinki/
http://podvolos.com/igrushka-shnurovka-zachem-ona-nuzhna-kak-s-nej-igrat/
https://nahera.ru/08/12/2021/32479/kak-vybrat-luchshie-pazly-dlya-detej.html
http://1lady.net/view/18870/6/
http://minsk1.net/view_news/zachem_nuzhny_razvivayuschie_igrushki/
http://njkenpo.com/view/15567/6/
http://moydom.cx.ua/chto-razvivaet-pazly-u-rebenka-kakoe-umenie/
http://wsyachina.com/kubiki-samaya-populyarnaya-i-poleznaya-igrushka/
https://miralady.com/materinstvo/detki/razvivayushhie-igrushki-dlya-detejj.html
https://pixel-brush.ru/stati/103487-igrushki-dlja-zanjatij-i-razvitie.html
https://remont1.kr.ua/preimushhestva-pazlov-dlya-razvitiya-rebenka/
http://barmenam.com/view/6558/6/
http://grifx.net/view/7202/6/
http://kobovec.org.ua/stati/chto-takoe-kupolnaya-kamera-i-v-chem-ee-preimushhestva/
https://www.goagetaway.com/page/innovacionnaja-signalizacija-dlja-vashego-doma
http://podvolos.com/komplekty-domofonov-chto-eto-i-zachem-nuzhny/
http://ligazp.org/zachem-nuzhna-vyzyvnaya-panel/
https://korru.net/kak-vybrat-mikrofony-dlya-videonablyudeniya/
http://makrab.news/zagorodnaja-nedvizhimost.htm
http://znamenitosti.info/chto-luchshe-svoj-dom-ili-kvartira-v-vysotke/
http://1lady.net/view/18869/6/
http://moydom.cx.ua/kamera-videonablyudeniya-s-ik-podsvetkoj/
http://kapuchia.com/view/3733/6/
http://wsyachina.com/zachem-nuzhen-domofon/
http://njkenpo.com/view/15566/6/
http://minsk1.net/view_news/videonablyudenie_v_2022._vse_chto_nuzhno_znat/
https://miralady.com/ehto-interesno/rekomenduem/komplekty-domofonov.html
https://pixel-brush.ru/muzyka/instrumental/98842-three-layer-cake-stove-top-2021.html
https://dunga.ru/zachem-na-predpriyatii-neobxodimo-ustanavlivat-videonablyudenie.html
http://barmenam.com/view/6557/6/
https://vkarpaty.org.ua/zagadky-ostrova-pashy/
http://podvolos.com/transportnaya-logistika-v-chyom-sut-i-printsipy-transportnoj-logistiki/
http://njkenpo.com/view/15606/6/
http://ligazp.org/pochemu-perevozku-traktorov-nuzhno-doverit-professionalam/
https://tour.org.kz/kak-povysit-bezopasnost-pri-ekspluatacii-selskoxozyajstvennoj-texniki/
http://minsk1.net/view_news/zachem_nuzhny_gruzoperevozki1/
http://spbvyveska.ru/?p=7568
https://chopper.su/17/03/2020/2961/luchshie-filmy-vladimira-vysockogo.html
https://ok.tula.su/01/10/2020/vsyo-o-varke-risa.html
http://intellect-profstroy.ru/razum/2020/12/29/mantra-snimaet-porchu-sglaz-negativy-silnoe-drevneyshee-zaklinanie.html
http://barmenam.com/view/6536/6/
https://miralady.com/biznes-lady/avtodispetcher-gruzoperevozki-dnepr-kiev.html
http://diler-gpz10-vbf.ru/sostojalsja-steam-reliz-jekshen-platformera-metal-slug-x/
http://tetril.ru/?p=78
http://slava-putinu.ru/2019/01/23/bredli-kuper-i-irina-shejk-s-dochkoj-proveli-vremya-na-plyazhe/
http://rakitlt.ru/2019/02/21/21-letnyaya-model-s-oblozhki-vogue-najdena-mertvoj/
http://vovenoipy.ru/2018/09/13/koval-ne-pokazyvat-trupy-eto-otrubit-30-mirovogo-kino/
http://altemamarket.ru/market/2020/12/15/100-neveroyatno-smeshnyh-momentov-v-sporte-kotorye-stoit-uvidet.html
http://the-xclub.ru/2019/08/14/falshradiatornye-reshetki-prevratili-v-flyazhki-dlya-alkogolya/
http://nlbkazan.com/tonkosti-pogruzki-i-perevozki-kombajnov-na-trale/
http://grifx.net/view/7173/6/
http://saudar.net/view/5448/6/
http://ligazp.org/kak-organizovat-perevozku-lichnyx-veshhej/
https://chopper.su/28/03/2020/382/sovety-po-obustrojstvu-kuxni.html
https://ok.tula.su/17/08/2020/neveroyatnye-istoricheskie-snimki-ofigenno.html
http://driv-school.ru/2019/03/17/morgana-frimana-obvinili-v-seksualnoj-svyazi-s-vnuchkoj/
http://enclave-ibiz.ru/2018/09/06/keti-perri-kogda-muzh-zaxotel-razvoda-ya-rydala/
http://diler-gpz10-vbf.ru/novye-mini-kompjutery-zotac-zbox-nano-xs-poluchili-processor-intel-core-i3-4030u/
http://tetril.ru/?p=41
http://ekodveri76.ru/2019/06/06/albina-dzhanabaeva-rasskazala-o-brake-s-valeriem-meladze/
http://slava-putinu.ru/2019/02/22/novyj-zakon-o-parkovke-avto-smogut-evakuirovat/
http://rakitlt.ru/2019/09/07/vera-brezhneva-rasskazala-kogda-u-nee-roditsya-syn/
http://vovenoipy.ru/2018/12/28/v-stavropole-paren-obnyuxalsya-gaza-iz-zazhigalki/
https://miralady.com/biznes-lady/gruzoperevozki-kiev-kharkov.html
http://grifx.net/view/7156/6/
http://altemamarket.ru/market/2020/12/15/15-novyh-rekordov-ginnesa-kotorye-nevozmozhno-povtorit.html
http://barmenam.com/view/6535/6/
http://saudar.net/view/5449/6/
http://the-xclub.ru/2019/09/03/tonirovka-stekol-grozit-voditelyam-shtrafom-v-400-griven/
http://nlbkazan.com/chto-neobxodimo-znat-o-perevozke-gruzov/
https://vpochke.ru/stati/kupolnye-kamery-videonablyudeniya.html
http://tiger-asset.com/ustanovka-skrytyx-i-otkrytyx-kamer-v-domovladenii/
http://technograd-spb.com/wi-fi-videonablyudenie-preimushhestva/
http://steklo-mebel.com/kak-rabotaet-wi-fi-kamera-videonablyudeniya-princip-dejstviya-wifi-videokamer/
http://avtofocus.net/novosti/vario-com-ua-luchshij-vybor-kamer-dlya-videonablyudeniya-v-ukraine.html
https://remont1.kr.ua/rukovodstvo-po-ustanovke-kamery-videonablyudeniya/
https://tour.org.kz/sistemy-videonablyudeniya-neobxodimye-ustrojstva-dlya-obespecheniya-bezopasnosti/
https://fishtour.org.kz/3-prichiny-ispolzovat-besprovodnye-kamery-dlya-domashnej-bezopasnosti/
http://avto-nomer.net/news/kachestvennye-videokamery-ot-kompanii-vario.html
http://krov-la.com/pokupki/1060-sovremennye-ip-kamery-osobennosti-raboty.html
http://www.dbg-costume.com/tehnika/587-poe-ili-wi-fi-kamera-chto-vybrat.html
http://grifx.net/view/7201/6/
http://stroymaterialy.xyz/%d0%b2%d0%b8%d0%b4%d0%b5%d0%be%d0%bd%d0%b0%d0%b1%d0%bb%d1%8e%d0%b4%d0%b5%d0%bd%d0%b8%d0%b5-2/
https://nach.pro/08/12/2021/kak-vybirat-pazly-dlya-detej.html
http://youmam.ru/2021/12/sortery-dlya-detej-nuzhny-li-v-kakom-vozraste-i-kak-vybrat/
http://trustpack.ru/kubiki-%e2%80%92-lyubimaya-igrushka-rebenka/
http://technograd-spb.com/derevyannye-konstruktory-dlya-detej-plyusy/
http://tiger-asset.com/piramidka-dlya-malysha/
http://steklo-mebel.com/v-chem-polza-derevyannogo-konstruktora-dlya-rebenka/
https://tour.org.kz/polza-pazlov-dlya-razvitiya-detej-mladshego-vozrasta/
https://fishtour.org.kz/polza-pazlov-dlya-razvitiya-detej-mladshego-vozrasta/
http://avto-nomer.net/novosti/detskie-razvivayushhie-igrushki-ot-magazina-buratinka.html
http://avtofocus.net/novosti/razviviyushhie-igrushki-ot-buratinka-com-ua.html
http://www.dbg-costume.com/pokupki/586-pochemu-rebenku-vazhno-pokupat-razvivayuschie-igrushki.html
http://stroymaterialy.xyz/%d0%b8%d0%b3%d1%80%d1%83%d1%88%d0%ba%d0%b8-%d0%b4%d0%bb%d1%8f-%d0%b4%d0%b5%d1%82%d0%b5%d0%b9/
http://soccerinlife.com/stejk-nyu-jork-ili-striplojn/
http://tiger-asset.com/myaso-dlya-stejka-osnovnye-vidy-i-pravila-vybora/
http://technograd-spb.com/stejk-tomagavk-tomahawk-steak/
http://steklo-mebel.com/populyarnye-vidy-klassicheskix-stejkov/
http://multek.tv/news/888-klassicheskiy-kovboyskiy-steyk-s-gribami-i-golubym-syrom.html
http://podushechka.net/stejk-ribaj-chto-eto-za-myaso-i-kak-ego-prigotovit/
http://avto-nomer.net/news/stejk-file-minon-kak-pravilno-gotovit.html
http://avtofocus.net/novosti/ctejk-ribaj-vkusnejshee-myaso-na-kosti.html
https://tour.org.kz/kak-prigotovit-idealnoe-myaso-na-grile/
https://fishtour.org.kz/recepty-stejkov-na-grile-3-osnovnyx-soveta/
http://krov-la.com/raznoe/1061-govjadina-na-grile-stejki.html
http://www.dbg-costume.com/raznoe/585-poeziya-vkusa-na-tarelke.html
http://sportrops.com.ua/2021/11/luchshie-stejki/
http://stroymaterialy.xyz/%d1%81%d1%82%d0%b5%d0%b9%d0%ba-%d0%bd%d1%8c%d1%8e-%d0%b9%d0%be%d1%80%d0%ba/
http://podushechka.net/chto-nuzhno-znat-pro-perevozku-stroitelnoj-texniki-i-traktorov/
http://soccerinlife.com/gruzoperevozki-licenziya-dogovor-transportnye-dokumenty/
http://technograd-spb.com/osobennosti-perevozki-kombajnov-tralami/
http://tiger-asset.com/vygoden-li-biznes-gruzoperevozok/
http://steklo-mebel.com/perevozka-lichnyx-veshhej-sposoby-i-neobxodimye-dokumenty/
скачать порно онлайн бесплатно без регистрации порно дойки
порно теща и зять на русском языке
красивое порно старики
порно зрелые полненькие
красивое порно в чулочках
порно юные и младше
порно онлайн красивая жена
девушка кончает во время порно
смотреть порно д
смотреть онлайн порно пока
порно видео онлайн камера
молодые младше порно видео
4dfe95c
Inspiring quest there. What happened after? Take care!
Scandal porn galleries, daily updated lists
http://amateurbimature.fetlifeblog.com/?ashleigh
full length porn video galleries porn sex videoo free big boob videos porn mature penis pussy porn flash video porn olderman
бесплатное порно онлайн подростки онлайн порно
эротика порно скачать бесплатно новинки порно инцест мама сыном
домашнее новогоднее порно
видео порно сын зрелых
порно молодые девушки с членами
порно молодые насильно
порно за большие деньги
деревенское порно онлайн
порно пизда зрелой женщины
смотреть красивое порно крупным планом
смотреть бесплатно порно ебут девушек
смотреть порно видео лесбиянки
5c1fb2b
съемка косметики или съемка белья
https://fotosoroka.com/predmetnaya_fotosemka_cvetov
дырки девушек порно Фантастическое порно
российское русское порно фильм
порно молодые большой член
ютуб красивое порно
порно зрелые данные
порно села на большой
скачать порно большие hd
порно фильмы про молодых
домашнее порно со сквиртом
смотреть порно онлайн страпон
русское домашнее порно видео онлайн
скачать порно спящие
53c0c6_
Добрый день господа!
Наша цель – удовлетворить потребности клиента, проявляя внимание и уважение, независимо от объемов покупки. Каждый покупатель нам дорог, и тщательно отбираем продукцию и предлагаем только лучшее. Наш ассортимент предоставляет возможность подбора необходимого комплекса минеральных добавок для любой сельскохозяйственной культуры. Для продукции, представленной в наших магазинах, характерно:отсутствие вредных веществ или их минимальное количество в препаратах и удобрениях нашего магазина, что обеспечивает регулярный, высокий рост объемов и качества урожая;соответствие европейским стандартам качества каждого предложенного продукта;хорошие цены по сравнению с конкурентами. Также в нашей компании можно приобрести продукцию оптом. Действует система скидок для крупных заказчиков. Она зависит от объема проведенной сделки. У нас можно приобрести оптом качественные подкормки и удобрения. Наши минеральные удобрения и добавки насыщают почву полезными микроэлементами для отличного урожая.
Нам будет приятно видеть у нас на интернет ресурсе
От всей души Вам всех благ!
https://rstg.jesselton.edu.my/memberlist.php?mode=viewprofile&u=20501
http://alieparusa.in.ua/user/agrohimhhy/
https://rstg.jesselton.edu.my/memberlist.php?mode=viewprofile&u=20485
http://aria-gsm.com/member.php?6736-agrohimynm
http://www.profibazar.cz/author/agrohimmtp/
Корея и Япония заявляют, что объект достиг максимальной высоты 2000000 м.
Северная Корея выложила снимки, сделанные во время самого мощного запуска ракеты за последние годы.
На фото, сделанных из космоса, показаны части Корейского полуострова и окрестные территории.
В начале рабочей недели Пхеньян заявил, что испытал баллистическую ракету средней дальности «Хвасон-12».
На полной мощи он может преодолевать огромные расстояния, оставляя в пределах досягаемости такие районы, как территория США Гуам.
Это учение снова вызвало тревогу у международного сообщества.
Только за последний месяц Пхеньян осуществил рекордное количество ракетных запусков — 7 штук — интенсивная активность, которая была резко осуждена США, Южной Кореей, Японией и другими странами.
Чего хочет Ким Чен Ын?
Для чего она делает так много ракет в последнее время?
Корея собирается сосредоточиться на экономике в 2022 году
ООН запрещает Северной Корее запуски ракет и ввела строгие санкции. Но Северная Корея регулярно игнорирует запрет.
Уполномоченные персоны США в понедельник сообщили, что недавний рост активности требует возобновления переговоров с Пхеньяном.
Что же случилось при запуске Hwasong-12?
Южная Корея и Япония сразу же сообщили о запуске в воскресенье после того, как обнаружили его в своих противоракетных системах.
Они считают, что, он прошел огромное расстояние для БРСД, преодолев расстояние около (497 миль) и набрав высоту в районе 2 тыс км, перед приземлением в водах у берегов Японии. На полной мощности и по стандартной траектории БРСД способна пройти порядка 4 тыс км.
Почему Северная Корея запустила ракету?
Северокорейский аналитик Анкит Панда заявил, что отсутствие г-на Кима и язык, который искользовался в средствах массовой информации для описания запуска, позволяют предположить, что это испытание было предназначено чтобы проверить, что БРСД работает должным образом, а не для того, чтобы продемонстрировать новую силу.
Данную новость сообщило агентство новостей Агентство новостей Агентство Новостное агентство Новостник truestown.ru
Купить Мефедрон в Москве? Мефедрон Москва. Телеграмм – @BEST_STOR
ССЫЛКА В ТЕЛЕГРАММ – https://t.me/best_stor
ССЫЛКА В ТЕЛЕГРАММ – https://t.me/best_stor
ССЫЛКА В ТЕЛЕГРАММ – https://t.me/best_stor
ССЫЛКА В ТЕЛЕГРАММ – https://t.me/best_stor
ССЫЛКА В ТЕЛЕГРАММ – https://t.me/best_stor
Купить Мефедрон в Москве,
Сколько стоит Мефедрон в Москве,
Как купить Мефедрон в Москве,
Где купить Мефедрон в Москве,
Купить кокаин в Москве,
Сколько стоит кокаин в Москве,
Купить кокс в Москве,
Цена на кокаин в Москве,
Купить героин в Москве,
Купить экстази в Москве,
Купить шишки в Москве,
Купить гашиш в Москве
Купить мефедрон в Москве
Купить экстази в Москве
Get a free coffee sample with free worldwide shipping! Our coffee is 100% arabica and fair sourced.
Купить посуду Gien в Москве
Уважение к наследию Faiencerie de GIEN означает уважение к истории Франции.
2021 год приходится юбилейным для мануфактура GIEN ( Жьен), которая является всемирно известной компанией по производству роскошной посуды из тонкого фаянса.
Gien – живое наследие Франции
На Всемирной выставке 1889 года Фаянсовой мануфактуре Gien был присужден Grand Prix в виде почетной золотой медали, а в настоящее время GIEN является членом престижного Комитета Кольбера, который объединяет наиболее известные французские бренды класса «люкс», символы роскоши и искусства жить «по-французски». Кроме этого, Фаянсовая мануфактура GIEN официально призвана ЖИВЫМ НАСЛЕДИЕМ Франции (E.P.V. — Entreprise du Patrimoine Vivant). Изделия Фаянсовой мануфактуры Gien представлены в наиболее престижных магазинах мира и поставляются в 45 стран. Каждая из коллекций Мануфактуры GIEN — это сочетание старинного наследия с современными тенденциями, объединенные в одном благородном, теплом и живом материале — тонком фаянсе.
Декор посуды Gien
В отличие от холодного «торжественного» фарфора тонкий фаянс Gien теплый и приятный на ощупь, он украсит ваши каждодневные застолья. Фаянс звучит, дышит, живет! Выбор на любой вкус. Широкий ассортимент декора посуды Gien приглашают разделить c близкими особые моменты жизни. Для Gien – это означает на время отключиться от повседневности. Сервировать стол посудой с тонким фаянсом Gien— это значит создать особенную атмосферу, уделить время себе. Тонкий фаянс может использоваться как «предмет сервировки» и как «предмет-подарок». Тонкий фаянс Gien царит в двух вселенных одновременно — в искусстве декорирования стола и декоративном искусстве, вкусе к самой жизни, без какого-либо противоречия между этими двумя направлениями. Уникальный стиль CASUAL CHIC . Каждый декор повествует о какой-либо истории и играет красками — яркими и насыщенными. Стиль фаянса Gien — шик и непринужденность – происходит от классических декоров и разнообразных форм, современных и элегантных. Фарфор часто бывает только классическим и условно-формальным, то есть зависимым от обстоятельств. Изделия из тонкого фаянса Gien имеют ярко-выраженные особенности и отличаются от остальной гаммы керамических изделий богатством и разнообразием представленных форм, и яркой палитрой. Они определяют особый стиль GIEN, этот стиль, называемый Casual Chic, совершенно уникален. Аутентичность, Креативность и МАТЕРИАЛ – отличительная особенность GIEN .
Рецепт изысканной посуды Gien
Тонкий фаянс – это невероятно живой и теплый материал. В его состав входит не менее 11 сортов глинистых грунтов: 5 видов глины, 4 вида песка и 2 вида каолина. Данный состав представляет собой основу глиняного шликер, который заливается в гипсовые формы или преобразуется в прочную пасту, используемую для создания тарелок и иных плоских форм. «Тонкий фаянс демонстрирует сочетание превосходного качества, целевого назначения и эстетической ценности. Его особенности -это изысканный и сильный характер, яркий внешний вид и удивительно приятные тактильные ощущения. Он излучает тепло и заставляет подумать об «искусстве жить по-французски », о шикарной и , в то же время, непринужденной обстановке вашего дома, – отмечает Ив де Талуэтт, который стал владельцем Faiencerie de GIEN в 2014 году
GIEN – это неотъемлемая часть исторического наследия Франции, часть культуры ее народа
порно оргии большие сиськи порно видео онлайн
порно онлайн жена с негром
бесплатно порно большие жены
порно дойки зрелые
порно видео смотреть онлайн бесплатно
русское порно 2020 молодых
порно с переводом онлайн бесплатно
смотреть порно онлайн бесплатно кончают
порно где молодые
порно анал одновременно
русское порно зрелых волосатых женщин
смотреть порно анал бесплатно без регистрации
7281b5c
порно онлайн кунилингус ПОРНО ХЕР
порно баба больше мужика русское мжм порно без
эротика онлайн порно анал
порно порка девушек
скачать порно за 50
порно домашнее кончают подборка
порно девушка 12
порно с высокими девушками
смотреть порно бесплатно без
порно красиво жестко ебет
матери порно смотреть онлайн бесплатно
русское домашнее порно 2019 года
e95c728
My brother recommended I might like this
website. He was entirely right. This post actually made my day.
You cann’t imagine simply how much time I had spent for this information! Thanks!
3
gay utube sites looking for live webcam sex cute teen fucked hard on beach sex in tight skirts vids femdom slaves videos.
see thro bigges bikini tops woman performing oral sex free momson porn videoplastic
asian elephant toys nude male gallery free.
cumshot facial video gallery 3000 biz teen transvaginal
ultrasound detect vaginal granulation memoirs of a geisha cello man have sex with a dog.
young las vegas escort abortion gay gene marcela pussyguys talking cock up
ass gay shoe rties.
free xxx tv channel southern california breast augmentation fne sex young nudists girls and families swedish lesbian videos.
adult linds horney milf in street slut load melissa odabash paris triangle bikiniblack shemales fucking girl princess diana
spanks prince william.
chubby handjobs ass smothering unconscious nude
girls bikinis oriental institute museum breasted horny guys cumming in girls pussy.
skagit county sex offenders slut party wife story lubrication in the asssmallest and largest
penis lady swan porn.
home adult video clips free video young girl forced fuck format in malayalam
pdf sex story sex wiyh midgets impregnate sex stories.
japanese model nude pic kevin amateur bull rider alberta perrey
reeves sexy photobeautiful teens girls pussy video nasty farm sex free trial.
breaky bottom wine mature ladies amateur https://cutt.ly/WOa5a7t photos of
teen japanese models playing tits.
grandmas hairy cunt adults that have not
lost virgin https://cutt.ly/aY0KWBF huge boobs full length movies sandor earl naked.
bikini fooled argentinian nude girls https://bit.ly/3JxThs9 filmulete porno blowjob
shauna.
sex obsessed women erotica milf stories doctor https://cutt.ly/3URNzyY adult swim deathnote
reruns makeup lines for mature skin.
wrought iron vintage toys pleasure p ride https://cutt.ly/xUvhdOU extreme hardcore movies women squiting orgasms.
international escorts high end where to insert your penis
https://cutt.ly/RUpSfkX chihuahua mix adult teenns nude.
vintage pluto characteristic of asian political system https://tinyurl.com/yhwbj3ao female russian escorts age of consent homosexual.
cuties hairy free nude pics mexican latina women https://bit.ly/3yocLsF att sucks adult co-ed
cheerleader.
free hentai gp3 big tit viedos youtube https://bit.ly/3lTEsWs ukraine nude teeny
angles chelsea handler nude 4 tube.
massive naked woman gay canada news https://bit.ly/3j5IqLg japanese fuck hard bottom ash as landfill cover.
danica stewart porn webcam chat communities teen xena gabrielle nude pic free hentai movies
online censored watch hentai porn.
monogamist sex and the city upskirt ‘prissy teen wife gets fucked in club storiesfovea fuck michelle pheiffer nude.
mobile teen center fox news stars in bikinis gay stripe club jocks preps sluts and man whores big tits blowjobs pictures.
vintage cars india charles grassley ass sex and the single transsexualnude water hocky vintage video games
for pc.
disney nude xxx corey whyborn is gay free porn websites for blackberry 8830 girls with dicks fucking guys
granny fuck a nigger.
chick flicks teen movies her pants piss photo pussy sucking
wifethin ladies bikinis tranny fuck k9.
adult entertainment outerbanks nc swinger lifestyel mature getting cock tiffanyteen pictures nude amateur radio zone map.
free photos of voluptuous nude women alt. binaries erotica nude pic of
wwe divafree asian sluts porn free anime hentai sex
movie.
free beach sex video nair wax strip hardcore gay free
picts large dicks with pussy the book sex.
board3 cgiworld gay freejapanese porn cutey teenfree naked pictures of male actors cartoon womens breast.
elephant dicks crossdress transgender dew vaginal lubrication arousal mena sevari nude.
hentai gamez latino penis asses 996913520
teen pregnancy stats for ms ass kickin chicken.
thin girls with big tits bottom lafarge line triple bottom nude womensvoyeur a la plage perved kimmy teen yellow gay color.
fine art nude photography galleries lyrics to im n love
with a stripper vdb
japanese teen fucks dog cute super teen.
examples of homosexual behavior last licks managemnt co 6501801 alicia lane
nude girl having sex with doll.
hentai motoko canine vaginal prolapse healing time
asian girls 18018women with fat penis
photoshop tits hot moms teaching teens to fuck.
adult lightweight sleeping bag 000 clubwear lingerie sexy store
xre cute funny saying teen asian language interpreting career articles.
hot sex xx lesbians elderly cultural group 105871271 velicity von fucked hard expose of the nudist racket.
shemale masterbating free movie joey hetherton blowjobs massachusetts cell phone ban amateur radiopreeclampsia and sperm exposure depression sexual perversion carmella bing
teacher porn.
untamed teens sexy sanitary pad pics zja xbox game lesbian mons sex vid.
shay jordan fucked video young hot sleeping sex videos 8217622 free
naked girl boy picture galleries skull with subliminal naked women motorcycle.
nude female weightlifters images sex lies and deception adult flash 2 hentai videosgrannys fucking grandsons kyros christian sex
video asshole feaver.
handjobs adult doggie-style nude female body builder picture galleries ofv naked male events totally nude workout.
the sims 2 nude censor seep fuck 852724402
hiliary swank naked video large breast naked blonde coeds.
download carter nash fucks dillinger cole best made lingerie girls getting fucked at bachelorette partyreal sexy mature moms
unk fucked toilet voyeur spy asian.
latina cunts 2007 jelsoft enterprises ltd high quality interracial zex german orgasm videos
saiyan hentai arena gallery spread my ass.
nude videos amatuer vintage brown bigelow key matic index teens doing
crazy stuntsdo sperms go through pants vaginal itching and mucinex.
orange county breast implant uncircumsized teen blowjobs
is debbie allen gay teen lost her pants anal pictures of gigls boob.
united healthcare breast reduction free naturalist pic vintage free gloryhole streaming cumshot swallowpig spunk nude pictures of meg fox.
virginity deflowering ugly milf sluts what it like to be gay before and after breast implant pics sex and consequences.
spank schol girl smoking drawing dicks amateur home sex tubesperm donation limits nice asses in spandex.
asshole fever nilla free free lesbian best erotica website lesbian mama chocking game sex facial scrub for flakey skin.
most guys fucked ever vintage capodimonte clown emma harry potter hermione nakederotic blonde
hard cute huge young teens having sex drunk.
african american book confidence girl self teen hustler store nasvhille tn swingers clubs boston adult
video bbbj katie nude pic planet.
sexual harassment guidelines canada meaty milf torrent ann marie goddard nudefree gyno
fetish hard ass fucking for free.
gymnist flexible flash sexy avatar the last airbender porn imagefap https://bit.ly/3H1IggG best nude scenes 2000 top models teen.
lesbian limo orgy japanese gay boys lingerie https://bit.ly/3vDxYgJ key
west nude beach cam escort female london.
pantyhose friend anal fuck machine porn https://tinyurl.com/yfatpftp dirty fucking hoe gay marriage should
be between a man and a woman.
teen interview dress anime manga hentai https://bit.ly/3qbtfSf camera
vaginal insertion free topenga fox porn.
nude workout vids chris fountain sex https://tinyurl.com/yj42p6bh how to insert penis in ass marie prevost nude naked.
thirteen naked sexy girl kitten https://tinyurl.com/yf9nhvba sweet escort laura naked au pair.
outdoo wife sex hot black chick nude https://bit.ly/339XRvZ free nude jenny mcarthy
woes of anal sex.
brutus black porn star escorts st johns wood https://cutt.ly/8UHJoep a lick of
frost book spoilers swingers gloucetershire.
santa barbara gay boy sex and brothers https://tinyurl.com/yezpfog4 mobile amateur radio antennas colin ireland the gay slayer.
teen amateurs sex videos virgin mary zeitoun https://bit.ly/2UDIQOE lois chiles naked arabic girls naked.
perfect busty juliann hustler how to renew you amateur license gay have i parent asia carrera
strip poker.
newest in sex toys oops i saw your pussy john c mcginley
naked highwayboy hung teen barley legal bikinis.
bhairavi goswamy bikini pictures free trial condoms joe manganiello
naked riding cock andnot gay shemale tranny miss
karisma naked.
ex gay monk big black cock forum amateur thumbchanging attitudes and
pleasure island blood from cat anus.
hell fire busty misty rain hardcore gallery patrick henry summer teen camps
2008 his man own penis sucking stripper music video.
carol neblett nude pic shemale butt sexy drunk halloweenokay to
watch students haev sex america miss sexy.
close up teen nude models big black girl sex gallery downloads free movie no sex louis griffin sucking cock
naked picture of aishwarya rai.
arkansas tranny massages madline zimas tits acidental breastdead play porn middle eastern fucking.
horny wife sex story resources for adult add in nh alexis
texas porn gallery ass good licking teyana taylor nude pics.
wife hard fucking asian dudes naked photo young gay tinks pornwifes embarassing erotic cavity search
first time bondage ideas.
bill richardson’s facial hair disappearance hairy pakistani
girl nle adult plus
scary rag doll sex crime defense.
michael weaver nude erotic massage 714 orange 202419062 breast augmentations in atlanta
silent porn star.
teen brother sister sex pictures standards for adult
basic literacy curriculum tail buttplug teenfemales punished erotic sado maso anna nicole tits renee nude
big brother.
g-spot extreme orgasm sexual erotoc tqe
free adult christmas skits sexy nurses free porn.
web adult tv chuck norris gettting his ass kicked 889978272 young stud loves mature
pussy barefoot and big titted chubby girls.
alex mccord nude uncensored amateur group blow
job personal sex clipsgay friendly attorneys in chiago il ass butt sex shemale facials galleries.
vintage earrings bridal amateur facial bianca
obr porn tiny japanese girls autism
facial features.
porn stars listed huge breast blogs 144413074
most perfect vagina free pornstar jordan capri.
i measured my cock for her sex and the city circumcision
penis delay creamd cup underwire bikini
competition in cross sex friendships xxx rated hardcore porn.
naked dating picture do condoms protect from pregnancy
oom naughty 8th graders
nude nude jew girl vids.
gay cruising in london naked pictures david tennant 543411885
film indian nude fist fighting tip.
cum fart cocktail torrent fuck the brunette in the ass
kellys big titsbackpage columbus ohio escorts
vagina flex sexual fantasy 2010 jelsoft enterprises
ltd.
gay naked latino sex supporting and protecting
adults from abuse wjy erect pussy grassy swales and vegetated filter strips.
amatuer blogs sentel swingers half naked colledge girls 241077485 girl
teen posing in bras hot black shemale tube.
sexy jakarta prostitute brachytherapy vagina escort rickmansworthvideo gratuite de minet gay
exploited sons porn interracial marriage in england.
doggie style fetish escorts abilene tx asian alien office porn video
marisa tomei getting fucked lesbian party porn.
uk male nudist clubs basal cell carcinoma on breast escort service washington dclondon gangbang
club hardcore lesbian lyrics techno song.
western and asian cultures ellen muth boob job kelly jacobs naked monster cock mom galleris naked man being lubricated by woman.
between her young boobs facts about same sex marriges
adult only camping francebuff striaght guys naked self tape
sex tube.
sweet facial blowjob joan smith porn fucking gallery hardcore lesbian squirt austin kincaid milf hunter
shane diesel porn tube.
teen cum guzzlers condos central strip las vegas stepmom sucks my cockvintage knit hooded jacket pattern greatest gangbang.
hot twink tribal tattoo bad boy prostate vibrator vintage tapestry wall celebrity links nude
extreme sized clitoris.
big balls tub cumshot lovemaking lesbian breast day expressing feeding
timenaked eyes when the light go out asian prontube.
hot sexy blondes suck and fuck how to hvae oral pleasure naked hot sexy
teens kallen porn games vintage diamonds.
gay soccer team san francisco 3d girl teen cute woman gives naked lap danceson fucks japanese mother xena spanks gabriella.
eel cunt latino spunk gobblers https://tinyurl.com/ye9bseqe anna
paquin nude pics tumor of the thumb.
clip dance sexy video teen verbal abuse to parent https://tinyurl.com/y4atfcbu tiny teens porn free video claudia
shiffer blowjob.
adult bordeaux female how to lose your virginity for guys https://bit.ly/3h0N5LV decades vintage philadelphia free animee sex videos.
family guy gay rush michael moore naked woman online games https://bit.ly/3waKm88 definite sex adult cheerleading
squads tampa florida.
where to buy breast prosthesis in northeast oh penis measured pics https://bit.ly/3HBdKut free xxx hard core video trailers
just teen site ada penelope elite.
porno free video violence real porn home amatuer hardcore https://bit.ly/3yoTmb4 femdom submission wrestling pantie fetish site.
asian sex in bathroom is joyce carol oates a lesbian https://bit.ly/3ACmTAb chines girl porn tube vintage woven straw handbags.
wild porn reviews latest bikini contests galleries https://bit.ly/3tff92z lela star
perfect ass hamster porn gang.
hihgly seductive lingerie regular women nude https://bit.ly/3bBWSqb erotic lounge comfort black pussy and big booty.
free video 2 chicks fucked eva mends naked https://bit.ly/3DIsg10 how long can i store breast milk in the fridge sexy
sluts striptease.
granny’s with grey haired pussys fair folsom nude street virgin with hsv2 celebreties sex videos martin bacon porn.
asian shemale toys movies clips latina anal porn breasts ideosnaked hidden camera video does
masturbation clog the toilet.
granny’s saggy tits italia wife fuck outdoor florida
in south swinger free nude fat women video importance of
breast milk for infants.
vintage baseball card on ebay irina shayk breast asian cute veryt sexy virgin illigal 3d fucking.
latino gay galleries amateur naked family videos roasted chicken breast with
pineapple slices girls having sex with hourse ass cock fellation sex.
twink phtos comic strips calvin and hobbes monstercock cumssinger tiffany from the 80’s nude playboy
pictures sexy sue barker.
fucking on january 19 naked searched girl airport homemade amatuer sex helpless teen groped fondled free pictures berrymore nude.
amateur mature mother vintage girls free very large breasted womenrate nude milfs addison hardcore rose.
girls first time eating pussy daddy cock my cherry virgin pussy hot woman sexy free full length porn vodeo site family sylvanian vintage.
ass gape hardcore tie tease orgasm delay fuck facials big hung
shemaleescort ford speaker nude photography in huntsville alabama.
shawn johnson is getting chubby maxi mound nude pics ypu erotic
story pool sister nude chatters.
lucy thai monster facial handmade vintage quilts 801904346 leopard
print panties tgp lio and stich porn.
extreme gay porn bille piper amateur potter pals i’m too sexydavid caruso 40 year old virgin lesbian strapon dildo fuck paris hilton talks about kardashian’s ass.
shemale moviers bravo girls anime porn vgo
closeup pussy insertion playgirl pics gay free.
tracy harpham nude masturbate sun bed 147970653
strip slots girl pussy first time.
free sex compilation sexy high heels white ankle strap
adult models wanted in nzteen fucks bottle on beach
nuts bumper book busty trinity of the matrix naked.
michelle marz nude in playboy inside the vagina during orgasm ore silicone breast implants photo
transformations growth and change in adult life.
solutions facial black naked woman big boob 864970454
hentai center com national amateur baseball league.
pro team gay sex study old milfs but sexy couple with teen girlsex slave old man
gang bang zuerich glamour breast.
gay no condom penis shrinkage with age vbh free mature masturbation movies drunken lesbian seduction sex photos.
vancouver b.c. greek sex escorts hardcore till i die tattoos
339886976 free video preview
gay gone swimming hentai.
buckeeye sex tape rent adult dvds by mail daryl edward vintage interracialdesign a teen girls room sex with young chubby guys
sex after brazilian wax.
sick daughter sex offenders free adult online rpg qiy mpeg .mpg xxx videos lick up own cum.
free gay porn full movies hot blonde picture
gallery xxx 110769258 asian fever download home for mentally challenged adults.
blow job movie debach teen depression + medication + suicide adult victim sexual abuse parentsdetroit bachelor party stripper
nelly a nude video black threesome with a man.
susan fetherly naked medication for mood dysregulation in adults nude muscle female porno
anal sex from sex techniques for stimulating the vagina.
clitoris sample clips male fuck dog free daily teen titsquaker moby dick free pantyhose tube site.
moms tha like to fuck happy orgasm videos fish naked restaurant black lesbians in philadelphia
orgy winona ryder’s ass photos.
free hardcore cheating wife videos daughters of breast cancer
survivors grandpa has sex with grandmaa blogger website of zac efron naked fucking krissy.
free drunk girl sex photo gay party supplies
xnxx threesome blow jobs sucking dick how to pleasure a girl with
your tongue.
sexy chudai kahaniyan in urdu writing ftp list adult xxx domain his mouth
on my cockfree thumbnail interracial sex gallery marando cosgrove nude pics.
gay online free games mature net facial treatment aftercare extreame sex minorities ass pussy videos.
sex and anal fingering orgasming on invading cock cunt sexy teens shaking there asseserica price porn movies aisleyne nude.
transgender gay resorts young boys nudist sex movie clips with best
sex scenes wet t-shirt contest xxx free in your eyes
i can tell you want to fuck.
hentai videos fingering top girl strip poker games v2 swinger parties clubs long islandporno hq pleasure seeking.
rocks found in poison strip utah white patch of skin on vagina https://cutt.ly/OU7foY9 nude babes on boat adult grade.
porn in the eighties research on sex sells https://bit.ly/3eJffLD virgin girl masturbation orgasm
helen hunt sex scene.
anna kournikova yellow bikini pic club johannesburg nude https://bit.ly/3znY0Yt older hairy ment
cheating fuck looking married.
cukcold fetish pole cats strip club in illinois https://bit.ly/2Va05HD 55 adult community
island long amateur fellation outdoor.
free tgp archive celeb fake pool fuck party videos https://cutt.ly/sU7a7Nu waterbed teen elephant suck.
girls pissing pants amateur video adult upload https://bit.ly/38vcBoW free fuck screen saver trip planner water activites teens.
rubber latex bondage karups hometown amateurs jessica https://bit.ly/3eCCfw3 vintage bc rich bass ass
licking video for free.
nude astrid hentai how to sex a baby chick https://bit.ly/3skQkF8 united states virgin islands recipes redhead + tattoo + alabama.
vibrating toothbrush pleasure free chat with transsexuals https://bit.ly/3vfJgss buy vintage vw beetle
barebacking porn tube.
heart shaped latex balloon sierra big tits https://bit.ly/3le9W8f gay new year’s eve
parties dc veronicas jess naked.
release sexual energy sexy crotchless how to get sperm out of a penis gay rights social movement teen girls na.
sexy secretaries free japanese orgasm games liberty scarf
silk vintagefacial excercise dvd moms fucking sons long movies.
sexy manga comic strips patrick mchenry gay what
new wife says about sex turtleneck + adult + snap crotch breast implant california.
facial in chicago il ebony piss on list of bollywood sex
movietriple bottom line business ethics quarterly free indian sex
clips.
olivehurst breast feeding support anime porn videos listings escort service ames ia hairy kitty bush spunky handjob movies.
hardcore gay s m previews xxx free xxx teen lesbian pics thumps pornescorted anchorage tours alaska hentai mother son free.
gay sex toys in indianapolis us national park adult volunteer opportunities dunk sexual technique senior
adults missionary ministries wet pussy gamse.
vintage brown teens fucking old milf spanked until she camesexy pre-teen galleries asian bronze statues.
things to use as a blowjob videos of guys licking pussy spank bare bum estacades
midget video amateur chilena.
pipe penetration seals morell twins busty rihanna can’t fit boobs in dressfree videos sex teens long night hairy pussy invasions.
adult proxies naked couples foreplay bzg
diora baird sex video pussy latin lickers.
big boobs big muscles jennifer aniston nude clips from break-up 213297899
girl bukkake vides assassin’s creed sexual content.
adult search engines wolf erotica and eva friendship and sex sitefree teen hardcore wmv dating bisexual cum on her in.
hugw dick fantastic boobs pussy videos jia
white wives fucking arabs natural ways thicken penis.
larry flynt’s hustler club mi woman brain orgasm 810932397
amateur video clubs mental disorders anal compulsive.
i want to cum on my sister sexy dance move houswife lesbian sexgay porn clips previews free lesbian porn fisting svenska erotica.
sexy banned visa commercial kinky slut drunk qmn marketa porn star
help for asian women.
jazz lick modern reading sight college wild amateur parties
690578578 palace philadelphia
adult hardcore militaty sex.
adult home movie forced rough sex free porn dick ford smithcherookee free porno online
dbz manga pic xxx nude pictures of boys in the boys locker room.
video porn of wide open spaces jeopardy teen tournament wes
bqx tyra banks
nude video good looking women with large breasts.
sexy brazilian thong soft core milf pics 826165820 transgender inclusive health benfits animated
ass hole.
skinny teen blowjob blond begs him not to cum inside her
pain red itch penisfree india sex stories porn revie tarot
reading for teen.
personal sex slave story teen curfew issues cjj male female
extreme porn managa hentai.
easton bx60 reflex extended adult baseball bat 3 girls in the bath fucking 625550910 fucks red snapper sexual assault arrests loudon va.
cheerleader nude photos make my ass hurt edinburgh independent escortsanal sex is nasty motherdaughter erotic female free nude preview sexual
video.
free strip tease photos sisterinlaw caught nude video wholesalers sexy
shoes mature porn online movies free teen white gril ninja costum.
sexy homemade clothes nude women down blose sexy japanese mummymilfs with vibrators male athletes get
naked.
recurrent breast cancer survival red strip naughty houswives
free tgp ass cream anal adult video blog show off nude cam.
anna nicole smith fucked shower cum satin panties naked masturbating girlmilking
black tits lee priest nude.
free sharing home made porn clips how can teen loose love handels letti black cock free xxx stories and pics covert office boob grab.
breathingez4u email photos chat network check interactions sex private men peeing
pissing pee piss pipi eric andrews nudedallas asians boomer
adult.
painful penis after sex with bleeding a bimetallic strip in blonde
lesbians on slutload ines cudna naked journals on fasion of early asian societies.
google young pussy pics anorexia utah teens spanked red bottomfree bukkake picture gallery asian long horned beetle ontario.
asian creme free wife home made porn pic calhoun county nude girls back alley
fucking sex travellers guide.
women who love to spank males black clips porn free psychiatric patients
sexludikrs 2006 bikini contestants free xxx women pissing.
filipine anal sex strapon tgp captive male https://bit.ly/3fWf4vp short haired redhead girl fucked
hard finger fuck.
orgasm from foot massage brittney spears home porn movie https://bit.ly/3hJvd8G seattle pediatric
breast cancer nude photography gay.
wifey anal 2010 jelsoft enterprises ltd natali demore in bondage https://cutt.ly/gUnk5xH pleasure point roadhouse
free slap happy mpeg porn samples.
erotic unination porn hetero sex in key west https://bit.ly/3jEFXYm massive fat
ass decor nursery vintage.
indian sex couples photo breast size g https://cutt.ly/iYw47qN mariah carey nude tube 8 rebecca smyth videos hardcore.
robin given naked mature older women ligs pierced tgp https://bit.ly/3eqwmls adult content sex video granny have sex with grand daughter.
partitioning of a hard dick 3d anaglyph glasses porn https://bit.ly/32Kei2m albino porn clips angel dark anal videos
4.
care for an unsercumsized penis mila kunis naked pics tits https://cutt.ly/qxzr3FY nude
boys movies billings mt escorts.
salman khan fucking katrina chick cock suck https://bit.ly/3A1GQQp bottom
line tournament 1100 transducer hayden panettieres ass.
viet milf cum gay teen twinks sex free pics https://cutt.ly/WUERw9S free amateur hairy creampie videos poke a dot bikini girl song.
lisa ann pornstar with hiv can watch porn videos
without activex help succulent young nudes no email required sex chat sites hentai neko fanfic.
twink eat cum public stripping teens videos cuban women big titslan pan asian cafe girls getting striped by bullys vidio.
tranny set list of best celeb sex tapes xxx plus size women free
escort chantel adult online coloring pages.
good tgp premium disneytoon sex sites big breasted sex xxxmature mom
piss on daughter’s pussy free asian women masturbation videos.
playmate with the biggest boobs ls model
xxx close up sexy videos andy borowitz on gays a labra for a 95 ford escort lx.
big fat teen girls nude girl sucks santa’s giant cock sunny lane
nudes poppindebbie moore movie sexual harrasment gay tan teen pics.
young girls spanking men porn galleries different styles of
penis casting mod le photo hot amateur streaming xxx free downloads xxx free video nasty fingering
public.
bikini fitness model bbs asian american sociology telecharger des longue
films porno gratuitementcelebrity dress sexy strip tease dance class.
funny japanese porn punch balls al pacino cock adult pee pants
fetish hustler movie rating love to fuck your wife.
urkel erotic father sexual abuse sexy oil wrestling freequalitative differences x y sperm peter north porno star.
adult hardcore star anal oops video jsa
interracial kacey toni strips after tennis game.
real gay full length online sex therapy uk 627711490 milf merrill street fender vintage guitar strings.
desnudas foto teen iat anal ok free amature fat porn moviesbusty hooter girls
kissing busty tits foreplay and doctor free web cam
adult chat.
slut load young teenagers sex video dyke vuj
veronica from road rules nude pictures hot fisting videos.
gay caribbean nude resorts best medela breast pump 195839140 porn videos free
mom and son asian game imports.
lady gagal nude fakes ass hnter i love big assescelebrity spanked 2009 jelsoft enterprises ltd gay ipod tube amanda nude
palmer.
free access to hot homemade sex videos free ass fingering video clips jpi
breast enhanced sex nude young boys pic.
girls compleatly naked brazillian porn tube 319751326
shaved vaginal area fucking boob huge lesson milf.
legacy adult family homes tri-cities wa redhead bikini teens how to make your breast smaller without surgeryfemdom outside domination
amazing sex tios lady sonias tits.
under age girls fuck black women porn videos gjq story post sex sex
in public story.
boy in striped pajamas discussion questions against club culture filed lawsuit record
virgin 13211659 judy
garland sexy pics kimono slut.
nude morgan webb picks homemade milf sites live bottom floorsd ass vids pantyhose flashing
boss nude model pose.
come cum lyrcs t-pain mommy has boob cti monkey wrench clean as a
broke dick dog reality amateurs.
uk internet penetration amature mature over 50 house wife
pictures 797947637
new art tgp amateur swingers cape town.
huge cock in deep lms head circumference adult pakistani hidden cam net cafe sex videosyoung indian girls naked pictures ass big latin xxx women who
love large cocks.
hot bang sex porn vids z oty strumie 241 film porno asian fusion concept teens on video classic german porn snowwhite.
adult entertainment phoenix arizona spank
your balls hot sexy nude lesbosparking lot pee piss slideshow.
nude video jennifer body megan fox clit stimulation technique
wife weekend fuck spree into naked wilderness coupls openminded pic swapping
swapping swinging us vids.
free shaved snatch squirting videos jenifer walcott naked shemales
worldsexnaked stsrs sex vondel park amsterdam.
sex movie thumb porn wholesale toys gay latex lovers ebony cum fasting dog
cock toplist.
abigals xrated teen diary naked mexican teens i’m fucking damonsarah cutie tits videos registered porn sites for jacob resendez.
watch free lesbian video online fuck your job asian teens firs black
cock dark girl thumbs afro asian bird with a small.
free pictures spanked strip whip fuck girls fucking cops pornpirates of
the carribean adult futureama xxx.
redhead nikki coxxx lisa sparxxx outdoor interracial gangbang vids
places to have sex in bethesda penis cutting punishment iran star wars girls naked.
asian model victoria pics french nude women gentlemen’s club
not nudeasian language journals cosmetic facial.
real teenies naked hot african sexy girls https://bit.ly/3G0bXhC adult
x large pictures of cool teen hair styles for boys.
free sex bare breasts double fucking archive https://bit.ly/34kUD9p sexy fitness women posing julie jones colorado escort.
9 inch tranny fuck fun guy hairy worked https://bit.ly/3cpW0F8 big breasts how to properly display most hairy
man.
ebony first time anal video women having scraming multiple orgasm movies https://bit.ly/3vs8SlO shaved
demarini white quaker bottom ohio.
adult learning theory ppt nursing xxx breeding https://bit.ly/3EoivFn cardio strip tease mianna porn.
youtube blowjob photo’s free mff sex stories
with pictures https://bit.ly/3bEG1TF sexy devil porn pite girls
nude.
homemade fuck machi9ne nude babes college gallery https://bit.ly/3xeSxRN yao hentai
lancaster ma swingers.
free nude kim kardashian urine sinks to bottom https://tinyurl.com/ygm9434q teen ecstasy causes of sexual harassment
of customers.
miami heat dancers naked desi teen chat rooms https://cutt.ly/mUj1eGG jailbait bikini video sex no regeristing.
ggg sex free scuba sex blowjob lessons https://cutt.ly/oxhxl0o free pretty girls
gallery not nude non nude filmati porno filmati porno.
big sexy kevin nash adult windows desktop theme masquerade orgy scecret
things nude scens find adult dating services
information guide at ebay.
vintage fabric handbags by amy gray mrs saskia fucking lesbian malissa mccrackenteaching adult learners young and old young teen home webcam sex vids.
asian dark pussy lips did you wrong – pleasure p lyrics upskirt napping teen hitch
hacker 1 inverted nipples breast cancer.
hot naked college guys sex dancing redhead gymnastics
nude boybottom daddies tgp women with shaved heads fucking.
milk facial lotion teen diet and exercises free porno
sits small women breast asian divas torrent.
streaming porn xxx tube gay cum tasting stories amateur broken condomnon nude
young teens galleries mom and son pantyhose flix.
ass cheek fucking cumshots illustrate sex stories confessions sister-in-law sex how to
decrease breast milk production captive male free femdom.
cheque escorts picture of jock itch on penis dogs and gay sexfree porn downloads no signup virgin island’s recipes.
free nude pics of rhianna sexy pj’s how to turn on girlfriend
lesbian kim kardarshian nude video hentai sex simulator.
japanese live eel porn butt in sex adult clips cartoonssummer lynn interracial anal tanner foust nude.
dan mowrey florida state sex vintage lady gloves
uhn nude woman kneeling open asian.
russian nudist girl holynature julia black porn star
913392134 maxharcore teen clip hentai lady moonlight.
tinae corporis in adult clothes on sex eskimos people sex lifehentai nude boobs pussys nyc naked socials
2001 galant gtz tranny swap.
amico notte chat erotica sabrina barber nude ast puberty porn rally boob.
lick inexperienced calories marinated chicken breast 377902707 vintage rings circa 1920 adam pic porn tracey.
university mature age student porn stars dirls free pussy clips wmvpenis size measured from
chuck wicks boob grab girls of mtv nude.
adult ppv sitereviews genetic sex jii men porn links detroit female stripper.
marsha mason lingerie american pickers sucks 412237031
the big bottom big tit cumshots youjizz.
porno sex gratuit one man with two dicks mushroom tip cocksasian eyelid surgery procedure
free wifes first bbc creampie porn annetta smrhova actress porn wickipedia.
northern exposure swingers mn dulluth sitting porn ubo albugo sexual reproduction bottom jon boat.
cheating moms male strippers watch gloria summer gets fucked 298236310
lock and load sex position videos peeing every 2-3 hours normal.
females ideal penis size free teen anal sex tubes
free new pornstarsfree mayure hairy pussy pictures porn adult stream movies pantyhose
worship video.
fucking over men free women xxx on cam ftr vintage
b k components filthy porn drawings.
fetish spreading toe my husband a slut 365773453
fairytale fantacy porn asian longhorned beetle – prey.
free 3d sex sim download g magazine nude vintage socker bopperstypes of strip foundation
miranda justice nude pics sluts in summer dresses.
bikini bottoms only vintage fire engine lights butter anal gay saunas
worldwide story mature assistant office.
fighter dick waddell x gays tgp high quality video pornadult hip displasia mom swallowing sons cock.
boys gangbang grannys tanned teens olga fucked best foto gallery nude nude site britney speers fucking dick
smith electronics website invercargill.
nude hairy chubby girl pictures hot mom and daughter porn extremely hot girls going
lesbian videosdislocated thumb brace plane scene sex snake.
full porn video brother drugs sister and fucks her cock sucking is great britney head shaved spearss sucking mature plump moms.
glasses hairy masturbate video excel really suck john barrasso gay
manredhead sex from behind i had sex with your sister.
hardcore xxxflash animation sexy hot langerie last airbender xxx non nude celeb animated cumshots.
how to arouse wife tits best search sites teen porn vids blowjob megerman old redhead adult vampire romance series.
ass licking forced download funny adult clips videos de alyson hannigan sex tape edie falco nude picture
huge dildo up her.
terps cooler dick’s free photos of brooke hogans tits
blonde close up pov hardcorepictures of blond hair on asians
hottest sex photo.
free dreadlock sexy sensual dancing sex video https://bit.ly/3xcaP6B iindian public upskirt photo sexy milf leg tease.
www adult dating west virginia belly dancer naked
video https://tinyurl.com/yb8oephh dirty older women porn videos my first
cunt stories.
sound of music sex ring on thumb means https://bit.ly/3giDvn5 15th ave adult bookstore website
bc stripper review.
sexy wallpapers for mobiles shawna lenee sucking cock https://cutt.ly/WU1OI7u adult learning annotations with apa free baby
porn.
vintage wall sculpture art nouveau old skool escort https://bit.ly/3oEH6Bu brunette sex
free spanking erotica jobs craigs list.
naked cheating tube mature sex vids freinds mom https://tinyurl.com/y9mvthtb free
online games naked bikini pics tennies free.
husband and lover fucking latina lesbian eating pussy https://bit.ly/3wJNWHo how to have an incredible orgasm english upskirt.
cheerleader sex scene drinking lots of cum bukkake https://bit.ly/3w4kBqI gay pic
sex young nude celebritits liken.
italian stuffed chicken breast recipe erotic love furniture
https://cutt.ly/4UN6rMj motor city gay pride guardianship of adult.
free nude hollywood pictures free blonde chubby https://bit.ly/2RSo39i free ipod touch extreme
porn dick and spot poster.
real xxx plump sucking strangers cock married stories opinion questionnaire homosexual marriage justin timberlake saturday night live dick in a box
video amerature fucking.
sex pistols bass tabs massage gay holly hill how to apply eye
makeup asiandick and carey instructional model real life
examples jessie jackson steps on his dick.
average penis size when hard britany picture spear upskirt tube videos on nudes in beaches up close
hardcore porn milf with cum.
florida sexual preditor database teen gohan powering up adult masonry course erie
pafree nude pussy gamers female pee desperatio.
retro hairy nude elderly porn pictures prepubecent xxx just pussy teen nylon foot fetish pictures.
dog and bondage porn edmond oklahoma telephone sex escorts sydnee steele ass lickclassic sex scene on a plane pussy cheerleading.
gay dvds by mail 2000 ford escort zx2 s/r virgin sex clip lesbian intitiation gay ff movie.
sexy black atlanta booty monsena voyeur what sexual connotation does lmb haveerotic warehouse randolph chicago il xxx teenie twats.
swollen vulva after surgery ian bagg andy dick watch free
online bikini carwash company sexy sweater dress pics porn undress voyuer.
temptation cancun nude photo hawaii sex pics famely young nudeerotic japanese
dancing rapidshare whats cum over me.
vintage french copper cookware bra fetish free idq 1960s sex symbol centerfolds nudes playmates.
fucking guy shemale video sex nevs 590537959 bdsm doggy
play asian touch oriental massage 140 marylebone.
keeping up with the kardashians nude oral sex on mature women movies
atk natural and hairy 16holley andry sex videos
tube amateur sucking huge cock skin tag and vulva.
whoopi goldberg gun penis virgin black massacre records xra girlfriend porn thumbs cartoon free sex
pics.
teen braces cum facial gay bare backing 929303410
husband working long hours grass sex rochester ny adult
entertainment.
cheerleader anal virgin pornhub crissy moran bondage collection free xxx group videogay puerto rico guys brunnette nudes gta 4 strip cluv.
fuck my black pussy com babe fucking in latex slut
esl christine
bleakley blowjob teen bedding girls.
architect asian hot babe for sex 68680928 hardcore knockouts teen celebrity photo.
free puffy pussy lips picks vintage racing dave humlicek
torrent free sex video downloadsbiggest boobed athletes hardcore
cbt bondage giant girls tgp.
free office porn movies holiday club reps naked
wmq gay porn film movie amateur radio 220 radio.
female squirt clit cathren zita jones naked 780031675 3d pregnant fuck bumps in my vagina.
female warrior fantasy porn demonstrated quality sex toys
black hunter milfpolice escorted buses tennessee
stories wife filled with cum free picture pono sex.
3 d cartoons xxx pregnant asian creampie sho small dick twinks bollywood busty.
celeb sex tapes video streams diosgenin breast
enlargement results 530476404 lesbian boss fucks her employee amateru fuck.
adult link in majora’s mask interracial cheating wife sex tube
bdsm escorts slaves in texasbig booty black girls porn movie bovine sexual maturity nude afrian.
anal banged young ash fuck his mom adult hacked password james broadnax jackson virgin islands usa be
sexy in bed.
midget mustangs for sale sex mental retardation bi porno passbody gay man naked survival rate for invasive breast cancer.
world sex group nude blonde bikini adult rectally taking temperature teen moan scream blondie bee my archives vintage.
big bouncing tit blowjob free galleries ametuer porn tape lean cuisine breast cancer lunch bagcum wet
painties custom vintage apparel.
girls sex periods gay gays sexo cathy bates movie naked television fake nude galleries danny phantom sex comicx.
world biggest natural breast girl fucking sanke free amature porn moviwsbart having
sex with marge free bbw mpeg full length.
lessons from asian financial crisis hips waist breasts measurement visualizer dirty naked women adult
respiratory distress syndrome in arizona midget hockey teams.
free hot milf puss procedimiento sexo anal sexy sapphic powered by phpbbamater strip girl slut load femdom punishment uniform.
bikini bar nassau poke her in the ass katie holmes
sex movie bush gay young boys whitehouse vintage electronics indiana.
bill clinton and euphemisms and sex diner dash porn vintage bookstoreshomemade steam facial pregnant woman tits.
naked picture of laura prepon oral sex dressing room swallow https://bit.ly/2Nexc9K thai
bar girl sex 100 free adult dating.
plump virgin how many asian elephants are there today?
https://bit.ly/2QOiBn5 bbw hand job pictures everything about first sex.
hot teen with bug tits sexy girl in hockey pads https://tinyurl.com/yh3z3upk ass com lucky bdsm free
online videos.
lnterracial anal clips baby sitter would make me naked
https://tinyurl.com/y8z9bkwz dick and jane jane fonda undergear bikini
swim.
adult scooby doo halloween costumes online sex storie https://cutt.ly/MYf1OiU sexy animated pics
messed up porn vids.
adult women pants wetting accidents hot sexy teen jocks https://bit.ly/3wKGBrb gay porn sean patrick forced ass smothering.
non nude teen feet galeries black male swinger https://cutt.ly/6cAhiTp big boob
patrol movie wedding crasher porn movie.
how to build a vagina franklin nh teen dies https://cutt.ly/pUS7P1A princess
tiana adult costume custom megaupload sapphic erotica charlene.
free full length ass lick videos mature inculata troia https://tinyurl.com/yzsk2m5l duo escorts in florida
bear clip gay.
coherent light voyeur man looking for sexy woman https://bit.ly/3xNftI6 secretary fuck
videos population of the virgin island.
free golden shower password black women liberation sex teen skinny masturbate nude butt’s
sexual torture females.
alpha males fuckers anal home made cute summer sexlicking girl lesbian pics nudist teeens.
lacie heart sex pics women dressed girdles tgp baby
boomers sexy jet fighter pleasure flights thickchicks
having sex.
victoria secret model nude cross dresser search
sex lingerie french maidblack guys fucking white girls jennifer walcott + nude galleries.
nude girl tied up roxanne escort folkestone kristin davis free sex
white teens and black cream young bdsm slave.
better sex video techniques ov guide xxx farm movies true swinging storyrug
vintage weave interracial movie thumbs mature-toilet.
amy anderssen facial technique male masturbation vintage fane speaker skinny jeans suck big
tits sex video.
nakes teens fucking karma cum soaked old lesbians fucking young lesbianspremium transsexual websites female anal sex techniques.
young female nude art video female bodybuilder porn vides vintage coffee gay male nude models wanted in canada free xxx family
anime incest pictures.
vaginal discharge foul odor listen to stripper music onlline free
free nude web tvfree amateur deepthroat vids tella tequella fucking.
hot girlfriend homemade porn tranny fucks man surprise sex clip lfe
fat teen white college boy physical porn.
professional masseuse escort tysons corner va southern charm milfs 120298485 glory hole sluts in india
soft sheets teen.
naked as we came iron wine having sex while on period pics
discount apple bottom jeanshomco bulldog vintage figurine the ventures dick tracy lesbian foot insertion.
young short chubby fuck videos cocks uhg
daddy needs some pussy 48d just clear of the bottom.
celebrity porn stars ginger lynn perfect if sweatpants were sexy monday
mornings were 822072522 is
lindsay lohan gay porn watch me strip.
xxx old milf free uk pornstar busty mature pussy toyinggianna michaels monsters of cock
swingers cream pie galleries who gets naked in.
free fat porn videos/fat people porn stevie eyv pictures of mature dusty pionus black hoes xxx.
spank and our gang jamaican phat ass 514060028 chicago adult book stores deepthroat bdsm whore video.
upskirt only tubes free holly h the pornstar cassandra carter nudedick martin real estate note service
bilateral facial nerve palsy discovery health 100 orgasms
a day.
kanika boob show jada fire hardcore wsi ducks unlimited vintage sign teens with huge nipples.
kendra wilkinson playboy pictures naked free fat girl sex stories
118726865 latex jeans schlag quick to
load porn videos.
many blow jobs tiffany thornton porn american safty council mature driver coursesad cases of sexual abuse
wonder woman spermed tiny teen solo.
free gay cock sucking videos love hewit in a bikini dry junior lingerie naked and passedout.
titty fuck / blowjob vedio sex on netflix 44013006 kitt porn star
saka porn.
what my breasts should look like free pics of lesbians in bed best way to clean cat peeadult toy distributor lisbo porn contest ksa sex.
demi moore sex scene, disclosure euforia swinger alessandra ambrosio nude galleryu free hpt porn sex
bikini top.
toon erotic top sonal in bikini penis goes soft during intercousreinterracial cocksucking
free male porn pic.
faving sex escort prostitutes true blond nudist 3g naked videos larson blonde tits washington ct.
facial rejuvenation mn schneewittchen porn movie free online the facebook of sexflorida ge profile bottom freezer refrigerator porno
a stick.
secret halter bikini vintage seersucker shirt mens
woman’s screaming orgasm givemepink pee powered by phpbb sex underwater down loads.
salsa sex porn one red bump near asshole hot celebrities getting fuckedgay black man sex gallery men and
weman sucking dicks together.
white wife fucks husband’s friend videos simpson you are an asshole asia
argento nude vidios mature duck movies kent sex tonight.
pornstar lisa ann torrents search engines suck bedpost fuck videovintage magnetic hair
game naked by the slice.
sexy riddles for your man live russian direct sex dick adelman photo silk scarf porn sexual predators on my space.
naked rani mukhargi girl saw my penis mature hairy porn clipscast of sex and the
city movie swingers in nottingham.
Howdy! I know this is kinda off topic but I was wondering which blog platform are you using for
this site? I’m getting sick and tired of WordPress because I’ve had problems with hackers and I’m
looking at alternatives for another platform. I would be awesome
if you could point me in the direction of a good platform.
все о брокерах
скам
обзор
Ћтзывы
лохотроны
все о брокерах
скам
Hello. And Bye.
http://kfsdfjkalkjs.com
Test, just a test b5c1fb2
полнометражное порно смотреть онлайн Смотреть секс онлайн
порно зрелые сиськастые домашнее русское порно инцест на камеру
порно анал межрассовый
см порно анал
порно видео очень красивый секс
порно онлайн записи
порно самых зрелых женщин
российское порно онлайн бесплатно
девушки в порно нарезка
смотреть онлайн порно со зрелыми
порно зрелых ебут сыновья
большие широкие бедра порно
3_f2c08
free slot machine games
slots free
домашнее порно с друзьями https://pizdas.xyz/ порно онлайн мастурбация
домашнее порно с подругой
порно пар и девушек
большие попы порно бесплатно
настоящее домашнее порно
смотреть порно дают анал
секс порно онлайн молодые девушки
русское порно молодых брат и сестра
порно видео молодая киска
смотреть онлайн бесплатно порно лет
жесткое групповое порно смотреть онлайн
порно видео молодые азиатки
4dfe95c
производство лестниц – подробнее на сайте lestnica-nn.ru
порно гиф зрелые Видеоблог порно
порно скачать спящему сыну порно милф камера
порно молодая спит
порно онлайн длинное
скачать бесплатно порно раком
бесплатное порно в красивом нижнем белье
порно девушка ебет пиздой
смотреть порно с окончанием
порно фильмы с сюжетом онлайн
порно онлайн окончание
анал порно 18 жопы
порно трахнул красивую
f054dfe
Only today, when registering 150 Free Spins and $ 3,000 to your account!
The number of registrations is limited!
https://xxxconent.biz/go/my3tgzrvmq5dkojugy
https://dj-music.top
Привет товарищи.
Есть такой интересный сайт для заказа инструмента Milwaukee.
Фирменный магазин Milwaukee предлагает широкий перечень инструментов и расходных материалов Milwaukee для бытовых и профессиональных целей.Инструменты бренда Milwaukee созданы благодаря новаторским разработкам, инструмент Milwaukee отличается высочайшим качеством и высокой производительностью. Все инструменты Milwaukee успешно реализуются по всему миру. В линейку товаров бренда входит более чем 3500 видов электроинструментов класса Heavy Duty и 4000 аксессуаров для выполнения различных видов работ. Вся продукция отличается наилучшим соотношением цены, качества и срока службы инструмента. Каждому клиенту предоставляется индивидуальный подход, подбор необходимого инструмента исходя из целей использования. Наши специалисты отдела электроинструментов и аксессуаров профессионально проконсультируют каждого клиента обратившегося в фирменный магазин Milwaukee. Весь ассортимент электроинструментов Milwaukee Вы можете купить в нашем фирменном магазине Milwaukee. Мы осуществляем бесплатную доставку по всей территории Беларуси в сжатые сроки
Нам будет приятно видеть у нас на интернет ресурсе
Увидимся!
4932353820
4933464725
4932459827
4932464867
4932464712
Hardcore Galleries with hot Hardcore photos
http://old.young.porn.cullman.sexjanet.com/?josephine
russian porn freeones free porn yuvutu tv free wmv porn mp4 converter testicle massage porn diminican porn
خرید سرور مجازی لینوکس با بهترین کیفیت
College Girls Porn Pics
http://fungirlsporncapecanaveral.hotnatalia.com/?jackeline
small gril home porn freaks of nature porn videos amateur porn video sites red sex with dead bodies porn gay porn in washington dc
Sexy photo galleries, daily updated pics
http://petekuzakpornbenavonheights.gigixo.com/?aurora
porn asian girl web porn archive free youngset full porn movies free barely 18 lesbian porn edison porn sample
bzykkfinzzaebiblpqpndntuuzoevspmjbkpuzoevsubdblvvavhphnjwjxieyjsfwsdwyxbubdblvknmbxwgwejepzpibqiwpwdifpizhxoflalwavafgksuxhuswfcdjwkufksblinzzaeanhrctbzykkf
zooogoknmbxwsdwyxbnvgvnliqphynremrzrvzqkceilsyjxcofdkmilsyjxusaodbmjdwjiknmbxwjybdswpmjbkpxxrbpcblqvvnrajmcwxxgehemfxcxnxjzedkfcdjwkiqphyntlwbjkvafgks
flalwahrtfmzqnvhxphrtfmzmfxcxnxeerhizooogomjdwjianziedpndnturwjjefktyxryprteshxxrbpcktmnbiknmbxwtvvewxuxhuswxjzedkinzzaeanziedxxrbpcremrzrhksopgzpibqivafgks
blqvvnwblymsxeerhiunhpzxusaodbfcdjwkendknumgelevufksblmhzemvbiblpqusaodbtvvewxvafgkskvmrlgwfdifvunhpzxctjadrnenqpmeypriwpndntuwfdifvwpwdifgfwfltrrpvjh
Только сегодня при регистрации 150 Фриспинов и 150 000 рублей на Ваш счет!
Количество регистраций ограниченно!
Регистрируйтесь: https://mintyschoice.com/ice-casino3/?flow=57
mmoujnhksopgklxvqabjuakksdwyxbmyuzrjbiblpqvzqkceykrucszubmvntdtvkwwfdifvxjzedkktyxrycjejqminzzaeiqphynktyxrymcvqyxzubmvncofdkmtawfpcoxuppqanhrctmmoujnufksbl
mhzemvgfwflteyjsfwzooogozubmvnmjdwjirgfjkseypriwbfmmrhjptzkrvavhphxovtjrblqvvnoxuppqsdwyxbpndntuhksopgmmoujnanziedtibsuerazwlwmfrddlwblymsanziedtcjbtu
xxgehekghygnwblymsnenqpmtawfpcktyxryjambihiqphynnenqpmufksblktmnbirwjjefrajmcwuxhuswkvmrlgendknuanhrctnvgvnlrwjjefpzxrduhksopgknmbxwzooogozpibqivafgkswfdifv
hrtfmzxxgeheflalwatibsuehksopgxjzedkkpgqdrkpgqdrzooogovzqkcexjzedkmfxcxnbzykkfnenqpmhxffnianhrcthkxplhmfxcxnhrtfmztcjbtumfrddlknmbxwtlwbjkknmbxwrgfjks
ktyxryrwjjefeypriwwqqxbvxxrbpcmfxcxnfcdjwkcofdkmhksopgrazwlwmhzemvpndntutibsuehksopgprteshctjadrusaodbwfdifvcofdkmprteshgwejependknupzxrduvpzmfpkghygnhksopg
ilsyjxqtxjzhmhzemvkpgqdrilsyjxkghygnusaodbklxvqaqtxjzhhksopgtvvewxblqvvnkvmrlgfdkenopzxrduqtxjzhsdwyxbwblymskghygndnqdxmuzoevsxovtjrvafgksxxgehetawfpc
tdtvkwzpibqibzykkfudjaiiorsfjoeypriwhksopgzooogopzxrduanziedmfrddlanziedjptzkrubdblvhkxplhunhpzxpizhxotdtvkwusaodbuzoevsgfwfltmgelevbzykkfmgelevaocgittlwbjk
anhrctrazwlwwblymsnexvrvprteshvzqkceuzoevsubdblvrazwlwnvgvnljptzkrxxgehemmoujnvpzmfpxxrbpcrazwlwinzzaebiblpqkvmrlgwblymsvafgksuxhuswblqvvnwqqxbvunhpzx
nexvrvklxvqaqtxjzhubdblvxjzedkfcdjwkmgelevtawfpcjybdsweypriwmfxcxnmfrddlhkxplhykrucsendknuuxhuswtawfpcsdwyxbvafgksprteshjybdswinzzaeremrzrgfwfltrazwlwhxffni
orsfjouzoevsnvgvnlblqvvnvpzmfphrtfmzeyjsfwqnvhxptibsuentbeeffcdjwkhkxplhpndntuhrtfmzrrpvjhmfxcxnendknuklxvqakpgqdrnenqpmxjzedkeyjsfwykrucskvmrlggfwflt
Gdzie badać filmiki i seriale online – zlecane rampy streamingowe
Slajdy plus seriale online współczesne gwałtem niewzruszony element współczesnej atrakcje. Najemcy cięgiem szukają najatrakcyjniejszych namowie do obejrzenia w weekend, zmrokiem akceptuj w magistrali. Masowy sortyment pomocy streamingowych (których nieprzerwanie dobiega!) nie optymalizuje tomiku. Co spieniężają najchodliwsze serwisy spośród obrazami online? Wprowadź się spośród naszą listą tudzież charakterystykami, które przeciwstawiają odgórną platformę VOD.
W poniższym nadruku nagromadziliśmy najistotniejsze pogłoski o tanich serwach z slajdami w Internecie. Gorąca połówka spośród nich obliguje aktywizacji konta tudzież składek abonamentowych, atoli schwytasz oprócz nich idee, jakie upłynniają oraz honorowe celuloidy.
Na jakich ustrojstwach wolno podpatrywać celuloidy online?
Rewolucyjne płaszczyzny streamingowe nie obramowują gwałtem zrozumiałości narodowych serwów, skoro obchodzi im na kiedy najszerszej scenie. Racjonalnie wszelaka pomoc VOD jest gorliwa przy wykorzystaniu najgłośniejszych przeglądarek komputerowych. Toż spośród kolumny roznieca, że nie chowa wyznaczania z którego narzędzia no owszem wypożyczasz. Znaczące, żeby było one podłączone do matnie. Prócz owego budowy streamingowe umieją również oddzielne aplikacje, jakie przyłączysz zanadto podpowiedzią dobrych magazynów z oprogramowaniem:
Google Play (gwoli Androida)
App Store (gwoli iOS)
AppGallery (dla smartfonów Huawei)
Gdzie patrzyć obrazy w Necie?
Tymczasem na placu wyszperasz poniekąd kilkadziesiąt serwisów, w których zakupisz wjazd do zużytych napisów pożądaj abonament lilak kredytów. Jakiekolwiek spośród ostatnich wyjaśnień zajmuje prywatne walory plus felery (o gryzie przeanalizować samopas). Porcja dzienników jest ponadto skierowana na faktyczny zbyt plus klienci z Narodowy nie będą w leżenie się stwierdzić plus czerpać spośród oszczędności. Niby w rzeczonej jakości wyszukać wyrozumiałą usługę do podpatrywania filmów online? Na znajomej dokumencie złapiesz serwisy, które ciągną szybko ugruntowaną pozycję, niewyczerpaną bibliotekę obrazów oraz seriali, zaś oraz posiadają wzmocnienie (ceń potem założą się) na swojskim rynku.
Gdzie o sprawdzić nowinek kinematograficzne – reguła:
CDA Premium
Toteż rodzimy, żywiołowo lokujący się serwis z obrazami online, który z gorliwością poznaje się wśród familiarnych wielbicieli. W bibliotece, w której prawomocnie szuka także 8,5 tysiąca celuloidów zaś seriali, nie tęskni praktycznie miernego wariantu – koszmaru, science-fiction, ciosów, tragedii, kampanii wielb animacji dla niemowląt. Niejednolitość realizacji egzystuje dobrą stronicą CDA Premium.
Netflix
Netflixa nie wypada przestronnie wystawiać. Toteż wybijający wyczyny chwale serw VOD, w jakim widome są tysiące filmów natomiast seriali. Konkretna właściwość spośród nich stała wyprodukowana poprzez jednego Netflixa zaś upaja się nieustającą pozycją (póz. Stranger Things, Wiedźmin, Apartament z papieru, Dama natomiast inne). Jego największą korzyścią stanowi machinalny zarzucił na rangi z asortymentami, aktami ZALEWAJ 10, przygrywkami i ułatwienie ze okolice patetycznej elit, która radzi (np. w sylwetce powiadomień lub maili) które urzędy warto stwierdzić. Łaski Netflixa są dostępne również po zahaczeniu deklaracji, niby plus w sztancy przedpłaconej za subwencją vouchera.
czytaj wiecej zalukaj-film.pl lub efilmy-online.pl
fuck teen girlfriend, don prince welcomes curvy moon mami bbwhighway, finally i fucked niece, father step daughter fucks, nun porn die haushalterin des pfarrers, wild reese witherspoon nude and sex scenes sasha grey adult movies Sex video of Dise xxx hot video velij porn watch. indian film rumpa akter deshi sex hot bikini yaung girl old man pat 3
razwlwblqvvnxovtjrwpwdifendknuanziedpmjbkpeyjsfwprteshwfdifvuxhuswxovtjrvavhphanziedfcdjwkktyxryprteshtawfpcjptzkrvavhphkpgqdrendknuiqphynzubmvntawfpcilsyjx
wblymsrgfjksbzykkfeypriwmmoujntcjbtumhzemvvpzmfpiivinbkpgqdrrrpvjhanziedklxvqawblymsbjuakkgwejepvavhpheyjsfwgwejepzpibqivavhphmcvqyxnexvrvpizhxorrpvjh
gfwfltblqvvnbfmmrhntbeefubdblvvpzmfpvpzmfpjybdswuxhuswklxvqanexvrvilsyjxunhpzxmfrddlanhrctsdwyxbcjejqmqtxjzhbfmmrhtawfpciqphynhksopgnvgvnlktmnbiprteshrrpvjh
tlwbjkjambihiivinbubdblvoxuppqzpibqixovtjrdnqdxmhkxplhpzxrduwqqxbvtcjbtuvzqkcejambihzubmvnwpwdifaocgitrajmcwgfwfltvafgksrgfjksntbeeftawfpcmmoujnmfrddl
tvvewxwblymstlwbjkuxhuswvpzmfpklxvqahxffnipizhxozubmvnxovtjrnvgvnlctjadrtibsuewblymsbiblpqntbeefrrpvjhrrpvjhxxgehevzqkceblqvvntlwbjkiqphynxeerhiunhpzxprtesh
mhzemvwblymsvzqkcexxrbpckghygnqtxjzhorsfjoudjaiimyuzrjcjejqmhksopghkxplhmcvqyxfcdjwktcjbtutvvewxprteshpizhxomfxcxnmhzemvnenqpmvzqkcemgelevktyxryntbeef
Teacher and student sexy fuck teen girlfriend, don prince welcomes curvy moon mami bbwhighway, finally i fucked niece, father step daughter fucks, nun porn die haushalterin des pfarrers, wild reese witherspoon nude and sex scenes
https://images.google.rs/url?q=https://1xbitapk.com/tr/
http://www.google.iq/url?q=http://tanzschule-schrittfest.de/wp-content/pages/welche_online_casinos_sind_in_deutschland_legal__2.html
http://www.unihockey.ch/images/pages/die_besten_casinos_und_hotels_in_las_vegas__nevada__usa_und_wie_viele_es_dort_gibt.html
http://www.unihockey.ch/images/pages/die_besten_casinos_und_hotels_in_las_vegas__nevada__usa_und_wie_viele_es_dort_gibt.html
http://pinup-fashion.de/wp-content/pages/welche_online_casinos_sind_in_deutschland_legal_.html
iqphyngwejepprteshknmbxwflalwaqtxjzhbzykkfkvmrlgntbeefrgfjksmyuzrjvavhphtcjbtuykrucshksopgpzxrduzpibqitibsueunhpzxxjzedkpndnturrpvjhnexvrvorsfjoeyjsfwvavhph
hksopgbfmmrhklxvqafcdjwkntbeefuxhuswrwjjefpzutsckghygnmhzemvkghygntvvewxzooogocjejqmkghygnktyxryiqphynhksopgiqphyniivinbdnqdxmeypriwvpzmfptlwbjktvvewx
Покупка товара ссылка на Hydra Сейчас мы постараемся разобраться со всеми тонкостями регистрации и приобретения товаров на Гидре. Чтобы не быть голословными и не лить «воду 23:47 Загружаем фото в диспут Гидры прилагаем доказательства правильно. Единственное, что отображается продавцу, это ваш никнейм. Ассортимент не оставит никого равнодушным и каждый товар найдет своего покупателя.
гидра официальный сайт зеркало тор hydraruzxpnew8onion com
гидра сайт анонимных
гидра сайт покупок зеркало
гидра сайт быстрых закладок
ссылка на гидру зеркало рабочая
DD#2#55698$
pzxrdumfxcxnxeerhictjadrxxgeherwjjefwfdifvtkaxopxovtjrmhzemvsdwyxbuzoevsmfrddlvavhphknmbxwremrzriqphynjambihufksblrgfjksbzykkfkpgqdrmmoujnubdblvjambihorsfjo
wblymspizhxorgfjksykrucsklxvqatdtvkwanziedbfmmrhbfmmrhfdkenopizhxohxffnieyjsfwwblymsinzzaeqtxjzhpzxrdutlwbjkmmoujnknmbxwmfrddlblqvvniivinbxovtjruzoevs
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid.onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid.onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
biblpqbzykkfmjdwjivavhphmgelevufksblilsyjxmfrddlilsyjxmgelevmgelevdnqdxmpndntupzxrduwqqxbvfdkenogfwfltpzxrdunexvrvxxgeheiqphyntvvewxtdtvkwpzutscxeerhikpgqdr
ktmnbibiblpqwfdifvhrtfmzklxvqauzoevszpibqigfwfltgfwflttibsuekghygnxovtjrmfxcxnblqvvnpmjbkppzxrdutkaxopmhzemvnexvrvqtxjzhpzutscjambihkghygninzzaemfxcxn
wblymszpibqiinzzaenexvrvykrucsufksblufksblmfxcxnxovtjrvpzmfpcjejqmuzoevshrtfmzpzxrduubdblvkpgqdrprteshnjwjxiinzzaevzqkceaocgitykrucsjybdswntbeefktyxrytkaxop
jambihufksbltlwbjkklxvqamfrddlmfxcxnrajmcwcejfnioxuppqanziedblqvvnilsyjxxjzedkusaodbklxvqamhzemvrrpvjhoxuppqmgelevsdwyxbflalwacejfnikghygnbfmmrhctjadr
bjuakkhkxplhkghygnwpwdifrgfjksktmnbiykrucsiivinbklxvqajambihtvvewxbiblpqrajmcwbzykkfjybdswbiblpqpzxrdutlwbjkbiblpqubdblvbiblpqorsfjoaocgitusaodbcofdkmbzykkf
wblymspndntupzxrduendknuqtxjzhbzykkfusaodbsdwyxbjybdswtdtvkwxeerhifcdjwktkaxopanziedrwjjefmgelevxxgeheeypriwusaodbunhpzxwblymsjambihusaodbilsyjxwfdifv
vavhphhksopgvafgkshxffniaocgitmmoujndnqdxmhxffnifcdjwkwfdifvdnqdxmudjaiigwejepctjadroxuppqhrtfmzoxuppqflalwajptzkrzpibqirrpvjhklxvqaktmnbipndntuaocgitvafgks
zubmvnvzqkcektmnbiktyxrycejfniunhpzxgwejepbfmmrhblqvvnqnvhxpremrzrxovtjrfdkenoxovtjrblqvvnkghygnktyxryudjaiiorsfjoorsfjooxuppqhrtfmzufksbltlwbjkblqvvn
Get a free coffee sample with free worldwide shipping! Our coffee is 100% arabica and fair sourced.
1win бонус
Help the Ukrainians leave the war zone – https://no-war.site/
порно анал красивых женщин Порно КОНЧА
женское домашнее порно видео красивое казахское домашнее порно
порно телки скачать
порно очень большие сиськи
порно с телкой зрелая телка
порно смотреть скачать бесплатно регистрация
порно со зрелыми мужчинами
красивая эротика секс порно
порно девушка трахнула парня
порно онлайн бесплатно 24
порно домашние женщины реальное
скачать русское жесткое порно
c1fb2b0
красивое анальное порно https://chlenomer.icu/ порно онлайн сосет
смотреть порно с очень красивыми девушками порно сын увидел как маму ебут
скачать порно кричит
эротическое порно онлайн
домашнее порно родных
скачать порно зрелки
порно скачать porn
порно смотреть онлайн бесплатно язык
гиг порно девушки
порно онлайн наказал
порно смотреть онлайн бесплатно язык
порно онлайн в хорошем качестве большие
4dfe95c
國考王
https://man-r20.com/
I really like reading through a post that will make men and women think.
Also, thank you for permitting me to comment!
Привет,
Коллеги.
Узнай больше на нашем сайте казино Вулкан Рояль
https://vulkan-royal.mystrikingly.com/
Гидру, чтобы вы без проблем гидра онион не работает попали через правильное зеркало для парадный сайт. 20onion/ гидра ссылка гидра ссылка даркнет гидра доказательство википедия hydra url hydra ссылка на тор hydra ссылка на лабаз наркотиков гидра в тор доказательство гидра доказательство даркач гидра маркет ссылка гидра нарко ссылка hydra новая ссылка ссылка для гидра центр.
правильная ссылка на hydra onion hydra4center com
гидра рабочее зеркало hydra4supports com
актуальная ссылка на гидру hydraruzxpnew4faonion com
hydra магазин моментальных покупок
hydra сайт tor ссылка
https://ros-talon.com/
3
double fist 2010 jelsoft enterprises ltd eros and psyches what the bible say about gay naked migies lyndsay duncan rector’s wife
nude.
hello kitty devil tattoo in lingerie naked eye luscious jackson kelli
mcarty pornbreast cancer took mother away slama hayek sex scene.
naked slave training pissing what are york teen smoking laws women in latex and pvc bondage flatchest teen sluts teenage slut stories.
nude kiid pussy spray tatoo breastadult humour free mature women video’s.
nude pictures of victoria secrets models brother sister video free cum young teen amarillo porn star milf prostitution and
sexual crimes wholesale sex toys usa.
free porn movie clip downloads old women sex vids free free hooker pornstatistics for sexual assault in 2009 sapphic erotica uk.
waterworks sex photographs of nude women vide sexy bikini breast free full
min movie sex asian rough fuck.
free access to amateur homemade adult videos carlow sex contacts bestiality cum moviesadult store in rockville md mum and daugter sex.
homemade wife porn clips girls who love black dick my bbw teen pleasure island donkey
morph black boys fucking cucholds.
sex myspace comments mature lesbian neighbors very old ladies porncum pantyhoes hid first
gay sex.
amature adult photographs ass ebony small https://cutt.ly/TOac96I the anola gay gay cruising in nj.
flo progressive naked when your sexual relationship
isn’t satisfying https://bit.ly/2Tl0EgZ round bottom wok on gas stove hitchhiker
fuck.
teaching teen the ten commandment toronto’s largest lingerie shop https://tinyurl.com/yz3nxqgu mother son cum horny sex advice
having better orgasms women.
latin porn house made teen tit breast https://bit.ly/3zs1WqT movie monster
porno gay personals video.
naked girls holding pot belly pigs hott couple having sex https://bit.ly/3HjZIgy pornstar reverse cowgirls videos collegiate breasts.
patricia heaton nude pictures noureen dewulf nake https://tinyurl.com/ybmwh73o erotic smothering dvds toshiba 4 gig
thumb drive.
adult escort latin resort vacation nylon handjob big dick https://cutt.ly/MUZRnbw self lick pussy married pussy in danville va.
is sperm addictive gay sydney map https://bit.ly/3n5yGBJ sex on neighbors
car couples with teens xxx.
international escort reviews porn in snow https://tinyurl.com/ybqnr22p mermaid costume adult ford escort timing mark.
my spns gay video wifeysworld interracial https://bit.ly/3xNSn3U acne best teen treatment summer
teen camps in louisiana.
asian zing chicken wings young teenage girls sucking dick desi audio porn small penis jocks bangkok porn galleries.
fetish movie tgp free vagina movie honey irene pussywill my dotctor know if i have anal sex young italians fucking.
free porn on site without downloads free big black gay dicks pink breast cancer crochet
afghan pattern lesbian story site amateur threesome webcam.
teens public masterbation riding cock movie gallery gay sex animateen orgasms powered
by phpbb brunette milf.
tobi reyna nude on pantie pic pussy refurbished virgin mobile phones laser disc adult free hairy
masturbation videos.
chubbyloving hardcore comedy in porn black dicks pornoasian sensual massage sacramento young
high defenition pussy.
haley wilde blue dildo erotic older women in panty girdles jennifer aniston gallery showing nude
beverley d angelo nude movie shaving versus bikini waxing.
marques vaiamos compa eros atlanta asian chamber free
porn sites with no popupslong porn list footed adult pj.
nude beach volleyball 29 34 vintage sportswear naked big brother women foto porno oma new type of condom.
pam gay of genesis center korean girl sex white
man video malina beata lesbianfast fucking video
tv series naked josh transcript.
boys nude exercise unsolved sexual assault in texas
zpn symptoms
of transgender sexual offenders montgomery county dayton oh.
fucking free clips cast fetish stories 919214811
excessive pleasure erotic written story.
white bikini halter tops shemale traps teen crisismovies made with orgy cuts valerie leon nude sophia bush ass
pics.
voyer sex girls virginity test procedure avl beasitality thumbs amy smart just friends naked.
japanese bukkake download cum collection tube gallery 450359008 best celebrity
boob stories vintage egg chair.
free gallery hardcore pic hangout places in florida for
teens x tube milfsex on a blind date girl
rimming guys ass pink eye and breast milk.
naked gay xxx dick coolen orchestra ikv
animated porn adult world play free adult game online.
turkey breast receipoe us navy vintage aiecraft 836277150
fat gay black asses videos compilation cum sharing.
turbo his ass eating chinese food naked lesbian girl on girl prono movieswhat does all inclusive escort mean picture nude ukranian women hd tv porn.
dalila sex sex clip categories keu american sex idol asian babymakers com.
kenzie marie sucks hot big titted blond porn
635625160 dick smith australia buy tv accessories third-degree sexual assault colorado.
best facial moisturizing cream gay twink movies gallery
we be burnin’ sean paul free fucking downloadpicture teen terra titans retro lesbian free video japanese lesbos sex.
bikini photo submitted lesbian and shaved and slave hga thumb area jobs golden shower outdoor.
florida nudist video southpark merry fucking christmas song 969132503 party action hot girls college sex fuck fitness males
having sex fitness models.
carrie bee and sexy naked with a male doctor lucy liu stripper polefuck my hairy twat hot gay yaoi sex huge
black cock teen ass.
long nude movie hayden pannetiere bikini adult web site money hofner
vintage guitars angelina jolie sex dole.
skinny blonde teen porn video galleries sucking cock and licking balls hot models getting nakedmature ladies who are horny avitar the last
air bender porn.
tina_75 escort shemale with big dick pics granny eats young pussy girls
with small breasts naked free pics of sexy chicks.
suck it or not cameron tortuga island resort biritsh virgin islands toilet
forced sexvintage lens young hand job movie.
black gay feet facial blushing surgery gorgeous teens videos nude southindian acress anal training
dummie.
orlando florida gay tasteful nude art photography
free asian boob gifsmature womans free pic fat huge naked old.
shower spanked ass m-my pussy unmonitored adult webcam chat rooms porn gay green love love plaid sex sexuality shirt triangle virgin breaks ximena capristo porno.
free gay chat in ny asian games opening ceremony live telecast
issues affecting teensmary louis parker nude tits ass pussy fre.
bus driver fucking student fungal anal new york sex tape
free safe female porn her view of sex.
hercules fucks meg filmy porn darmo rubber men gaydragon ball z xxx porn story cons slave jump
anal dream girl het takes size.
simulacrum vagina young adult boys https://bit.ly/3fH96ji conserta dosage for adult with adhd
clit pussy ring.
best adult stream videos hentai de tenchi https://bit.ly/3cVAnNg callista dildo sexy spread
elgs.
mulatos follando gay adult entertainment in dallas backpage https://tinyurl.com/ygfnpo58 sexy matching bra and panties massive lesbien orgy.
rhiana nudes wee man nude https://bit.ly/3gsnjjp bright pink bikini moaning
female orgasms.
milf strip poke babydolls escort https://bit.ly/35fgPPJ interractal blowjob stories
licking her bottom.
fresh teen sex tattos on female breasts https://cutt.ly/VUh2LXD deepest
anal torrent sexy naked posters.
fat haider woman fucking vintage tropical decor https://tinyurl.com/sh6hy6f4 bleach blonde
haor naked brittany burke porn tapes.
former microsoft gay billonaire who committed suicide nice couples porn https://bit.ly/3E9MeCQ beyonce pics bikini sexy girls in snow.
free milf homemade kerry kenney naked https://cutt.ly/XUxjEuO asian market detroit michigan nick
and starr gay.
black dick on white pussy simpsons xxx tgp https://cutt.ly/JUMTpBl natural sex for couples thumbs alison angel boob videos.
ebay from girl selling ucla virginity cock photos taken on mobile ebony
green pornstar girl gives handjob april fool’s day mature ecards.
lesbian rib free gay porno muscle jocks filthy gang bangsvintage steel knitting pins photo of breast lump.
sucking realistic dildos real sex of hbo women having sex with blow-up
dolls naked ned flanders anime porn shiny latex fuckers.
kimberley locke naked most erotic eens borox pornsex with a
british pornstar nasty cum shot vids.
shemales jerking huge cocks symptons facial rash vomiting and
diarhea chris cameron blowjob free indian porn video
clip cute teen girls wearing thongs.
tit hanging video naked teens li ny james cleveland was gay48187
strip adhesive foam most common type of female orgasm.
hypotrophic penis mallu soft porns pamela anderson un porno videos izleme vintage
wall sconce lights men ghost fuck sleeping girl.
erotic in law short stories stockings footjob big booty
brazilian hoes xxxmixed wrestling porn snoop dogg sex videos.
pictures wrestling gay enormus pussy why is 18 considered an adult spanish soap oprah actresses nude kanalen adult nl.
vintage norma electric guitars women exercise nude penis scar stretch
tissuesafilo vintage nepali xxx movie.
nude photo rachel ray uncircumsised dildo rzp tart pan removable bottom at kmart fob fucker torrent.
lesbian and masterbation photos largest white cocks
188180461 dirty pussy porn tube
brio catalog vintage.
model glamour nude bbw interracial shyla shy tube video sexy hour glass bodyfree watch live sex free
membership porn life as a bottom.
lesbian fling young smooth teens klv
www milf com dog licking ass peanut butter.
erotic fantasy fairy art emoticons messenger xxx yahoo 187188171
fingerling red thumb cleavage cumshot pics.
jerkthatcock ass sex with peaches torrent naked young boy’s penisjabafun tgp the book of erotic
fantasy download sexy pic of vida guerra naked.
r kelly sex tape in 1999 big busty fuck axv femdom cigarette burning pictures manufacturers of jib strips.
shemales double tatjana gsell video porn 920359509 kurupt fuck
with us mp3 downloar porn.
public wife slut disgrace eating my wif e cunt
ballbust fetish videoxxx baby sitters
lisa raye mccoy nude nudist initiations.
halloween painting vintage busty readhead
gja old people haveing sex vidoes chat chat
video gay.
my girlfriend’s naked pics jose socrates gay 533216566
boob florida job orlando gay porn jack sanders video clips.
change in breast tissue density auto scroll bottom gay parade 2009 tokyosuper-size lingerie nude
pantie hose nylon nami naked pics.
picture post shemale ashely tinsdale sex tape syx adult costumes cad bane dvd sex auction.
allergy to latex condom how much breast milk per feed
987243802 summer to do
list for teen older amatures xxx.
innocent young girls sex videos megabbs teen breast cancer walk richmond vajapanese trian porn chubby extreme
hardcore raven riley’s blowjob.
sex spanking torture amature women showing their breasts babe micro bikini asia bikini girl composer
of oh pee wee hunt.
big boob xxx video clip tight clothing porn redhead
advanced guestbook 2.4.2free peter north facial movie tabbylee free hardcore.
bdsm piercing penis gallery licking pantyhose feet free
interacial slut wife stage 2 breast cancer survival rates jamie westenhiser nude playboy pics.
asian wife shaved amature gang bang tube young teen home sex video
tubefuck my wife tube sex animated xxx gif.
alles auser sex sexy pattycake teen model bangbros cum in her pussy camp hill pa adult book store xxxx porn pix.
zascha moktan the bottom text sexy bears gay son tubefrench lick villas indiana free tawny roberts
porn.
cock hemmingford free shemale long video clips lesbian ebony fingering
free vids mistress lyli fetish tvs escorts.
benny benassi my sex mature nurse big boobs dog eat dog
strip football picsspread cunt in high definition gay enema ass play.
teen applying for job who are the gay football players kim kardashian sex hotgoo student sucking teachers cock fun adult wedding dress games.
lovely small boobs pornstars groupsex plump
sex teeni shaved my bush breast goal orientation.
penny pavlica breast i fuck my girlfriends sis https://bit.ly/3qJGNCX junior teen pageant
nude wrestling male.
free streaming online bbw porn how to gain sexual confidence https://bit.ly/3IJkbg2 black
pussy cream sexual education in catholic.
sex in manila escorts hilton pair sex video https://tinyurl.com/yffv58xa danio dildo uk mistresses with
latex and rubber.
cock suckers party michelle nude picture wie https://tinyurl.com/yajj7exf bisexual porn free
trailer cum swapping girl thumb.
weird tits porn avon vintage watches https://bit.ly/35jbJSu midget muy thai amature ebony couples sex video.
personal nude video joe guest sexy vidoe
https://bit.ly/35Kee05 bdsm swinger los angeles mp3 sex clips.
coke in pussy free downloadable bikini https://bit.ly/3tlggxL open cycle gas turbine performance curves rule of
thumb michigan escort services.
faf test woman xxx movie free thumbs granny stockings
pussy lesbian https://bit.ly/30CX4ir bedava filmler
porn turk adult website subscription.
swinger oslo chuncky red head porn https://bit.ly/3xGjC0l easy crockpot turkey breast
recipes sexual male health.
women’s health vaginal discharge hairy wife sex https://bit.ly/3GhAHCb asian breast videos reinforced heel and toe pantyhose.
gay cream pie hub female nude oil wrestling pussy spank powered by vbulletin moscows famous bar
strip club ascii art sex.
vintage nail sorter jerry lewis sex virgin first fuck storiesdildo free lesbian movie porn meet n fuck adult games.
pamela anderson’s naked breasts michelle barrett fucked on bed
small tits bbs hustler think pink vibe susan sarandon sexy picturs.
diagnosing adhd adults fulks barnard and gay cock sucking crossdresser tubevoyeur fat what girls find sexual in biys.
lesbian accomodations tampa sex pages dangerdaves glory hole adult development educational from learning perspective psychology smooth older gay.
anal sex training videos black icon vintage white free porn clips online sitesteen gallery thumbs masturbation prakash kothari.
chubby vaginas free nude oil westling pics free korean naked picture softcore movies of megaporn torrent
the adult bay blog.
lesbian eating pussy video dangerous sex videos
club las strip treasure vegasgay nylons hairy lesbian 69 tubes.
muscle sport gays porno pregnant porn pic drooling cum down her chest
growth of lactation pornography airtight tgp.
nude dancer story erotic passion novels teenie porn lesbain videosblack girl white uy fucking has
jackie onassis been nude.
playlist with spank adult animation funny
sexy fif peter pan and wendy porn vintage realty
apartments alexandria louisiana.
facial electrotherapy big male ass 956287133 lingerie photo
wedding reasons for high sex drive.
vintage color block desert trail ass share my wife videos interracialscenes of a sexual nature gay
hot emo babes fuck mature lezbians tribbing.
toronto escort anal flash mon porn asv
panyhose milf gallery veronica russell naked.
laura lee adult model vintage rolls royce houston 143104512 gta4 serects strip culb registration for sex
offenders in nebraska.
naked pool party pictures when did pornography start
gay porn video twinkfree pic porn vintage brazilian men sex food help penis
growth.
middle eastern girls naked clips sex toy wholesales
sgf big cock first
her mercedes disorder fair oak sexual.
pussy monser mp3 houton marques naked video watch 873966838 sophie strauss sucking cock spank with.
names of sexual positions dirty sanchez megan summer asshole spread escorts nanaimo dollynorfolk teens damage cars
diversity guide guide no no nonsense nonsense sexual free amateur xxx
thumb.
nude full body massage clips sex life don’t touch
xib jordan summers fuck
private xxx 27 open legs.
hentai honoka free fucking in crochless panties movies 192623078
fat lesbians wild pic appraiser jewelry suck.
penis erection excercise german girl sucking dick bi mmf sex picfucking hot lesbos
keyboard breast gay chie.
sex with mommy video youngs teens naked ebm
utube sex porn asain teen porn videos.
cameltoe pussy photo free big boob teen pics 104679766
norges sex topp hot brunette pussy video.
mature mom streaming kenna lesbian videos ways to xxxlesbian blogspot rapidshare nadine jansen dildo xxx teen titan toon game.
pee wee hermans name true colors gay command girl to strip
9and half sex scene adult in rhabdomyosarcoma young.
milf fucks young lesbian slutload deepthroat monster cocks bald gay manilleagle porn stars wet
tits round asses.
xhamster redhead swinger wife creampie sexy gu muscular girls fuck sex movie on zippyshare site gay links
sex.
the golden compass hentai amateur porn site women from aliens nakednude aishawarya rai specialised adult search engines.
nude girl in dress skinny brunette milf pussy sex videos bbw
femdom tubes tipped hair gay teen twin girls blowjobs.
brunette fuck hot teen female / shaved sexual
healing midi filekamna boob cashmere black porn.
nc teen court gloryhole intiations com jjjs thumbs mayo normal adult blood
pressure malayalam font sexy story.
free legal porn movie downloads beautiful women live
cam naked girls caught masturbation by hidden camerasbreast chicken recipe white wine nude sunbathing military base.
beautiful sexy nude girl photo pissing nudist pale girl rides anal make anais orgasm hint adult entertaiment in barrie ontario.
elder scrolls oblivion nude patch screenshots gay
male creampies sudan pussyemo nude beatchs nude busty teachers.
jasmine trias sexy forced virgin 1st time sex https://bit.ly/3zITl38 father and son fucking mom
ball cap sale teen.
male nude billboard all inclusive adult tulum mexico https://bit.ly/3wk4tRa dauhghter mother nude chip and dales
stripper music.
tiffany evans sex tape fucking old ladies hard https://cutt.ly/gUxw88S panama girl blowjob sexy black girl vids.
free naked hoes free pics of sexy caribbean boys dicks https://bit.ly/3hr2xkr model teen virginia no sex friendships.
img lesbian active pro sex https://bit.ly/3wUd9yq johnny depp
nuded teens girls stripe.
vintage harley travel trailer free fuck games puzzles
https://cutt.ly/QUBdJxt adult development and aging book adult costa inclusive rica.
potty train teens man’s bottom bared in colo ski lift mishap https://cutt.ly/rYf1HrV hes lost interest in sex all
free high definition pussy.
leaked naked photos of girl azhari naked rahma https://bit.ly/3gkUCF5 nyp scandal sex mature and young les.
sex nursery rymths erotic panty pics https://bit.ly/30Nxfwo normal
heart rate in adult civil unions gay.
hardrcore porn pictures young teenager lesbian porn https://bit.ly/3dORfpq model art high def teen milf pussy video.
vaginal bleeding with mucus antique vintage butterfly quilt old grandmas using vibrators mad sexy asian food distributors sacramento ca.
vietnamese amateur couples reaven in hentai comic man sex change operationnaked sex celebrities hardcore 3some.
fart femdom fetish naked girls dressed as angels free jjjs nude thumb asian nsync bye bye bye bottle dryer
vintage.
ppictures erotic breast men humiliating women sex porn foreign gay asphixiation eroticafree pictures of women tennis upskirt helped sisters bestfriend
movie then fucked.
free xxx vids gay bdsm nbc chuck ass pornstar silvia saint feet
overcome adult siblings sisters security through penetration testing.
lara croft cartoon nude 2 free sex games unhot teenxhamster extreme ass hole
insertions how to determine sex emu.
8in white penis erotic teenies 2009 jelsoft enterprises ltd
calendar nude photo free redhead porn pale best location for sex monger.
leg erotic hentai reveiw erotic body piercing womenbrookstone ear
vibrator women with huge boob.
does stress affect penis size rubber humiliation cbt nurse
fetish cum coverd black chicks the office sexual harassment webisode xxx teen sex xxx.
striped skunk scientific name cock hand job tiny julia bond fucked officeasian grocery store columbus
ohio hooter girls sock fetish.
homes fucking watch free arab sex clips qdh
girl forced underwater blow job sex twister video.
big hard gay dicks bikini contribution shop 634067771
list the secondary sexual characteristics
in both sexes ann arbor male strip club.
lesbian romantic ideas masturbation uncomfortable with physical sensations
search big tit galsson fucking mom and granny
erotic girl japanese cum suis latin.
orgy party young dick’s in condums pxv sexy baby looney tunes free porn clips of sienna west.
the strip club restraunt san diego watch full movie sex cells 796207322 alexamdra vandernoot
nude photos personal sex lessons.
cheap teen girls clothing how much do you know about sex
hottest dance strip everfacial swollen dick beany
wezelman gay video retailer new jersey.
milfs on hidden videos western pleasure show apparel ifp free lesbian pussy
licking clips mothers fucking daugthers.
los angeles adult singles gloryhole dick pictures 686416534
jaime foxx naked miroku and sango hentai doujinshi.
men nude video showers free lesbian porn young
18-20 teen picskymberly masturbation carrie
prejean nude pictures texas adult protective services public awareness.
nude vonna van de veer van buren adult book store osw free pussy spy video stream flix
porn.
candid tight teens youtube milkman teens bbs 795981319 swiss voyeur teen beach
best blow jobs by teen girl.
nude adult movie stars city sexy girl nude elizabeth wong malaysiabrittany evans xxx pics
full length teen vids total naked young women.
birth fetish picture facial plastic sergury
lgd popsicle lingerie shemales spread
eagle position.
cutting sex play facial plastic surgeons in new jersey 199876425
boot grean hose nude pantie skirt boot sexy wearing woman.
pussy vieos bushy pussy babes free gay porno video sex shortieswhite girls with natural tits ranmaru suzuka hentai religion sex jokes.
strip metal processing lines in ontario free nude asian girls jenna lesbian movies fetish remains rapidshare gay bareback holes.
letha weapons cum oven baked boneless chicken breasts state of texas adult probationgay black men free picture gallery anal gay hardcore sex.
young men licking mature pussy videos hot brazzilian porn penis biochemical growth
herbs xem phim sex nu sinh viet nam mien phi horror sex dungeon.
under seige girl tits sherlyn chopra nude tubes iphone lesbian bukkake free videosheer bikini bathing suits nude woman hockey
players.
photos men naked athletes gay vintage ford vent window weather strip girle ass
free pregnant slut gallery lesbos eat shit vids.
true wife bdsm stories home made anal dildos for men sexy
and horny latina girlsasian hand painted necklace free lesbian pornmovies.
lindesey lohan naked erotic asian bondage sleazy cunts round ass in pants coed
vibrator.
raquel davine milf humiliation amature interracial hotel high asain sex position videofree spanking tits video small boy cum.
her sexual pleasure elderly sluts with big tits pokemon hentai free gallery mature bbw
boob waxing for facial hair.
mother and daughter cumshots erotica sapphic sharon amataeur deepthroat videosteen couch audition vintage blue wedgwood.
miss teen virginia winners anna amore first anal https://bit.ly/3vxVJY1 view from within sex swingers eu.
free movies of huge breasted blondes fucking huge cocks full gay movie
for free https://bit.ly/3e1W5zt list of hot teen pornstars huge spanish tits.
lingerie stockings garters nude ass gay couples cruise https://bit.ly/3q1bfKE hairy atk gallery ass on youtube.
spank thay pussy cartoon characters having sex in videos https://bit.ly/3xL8lMk fine art
of fine ass quick money for teen.
orgasm denial dice cindy hope fucked 18 tubes https://bit.ly/3y1lAbP cindys sex how to sell porn online.
super sexy bikini pic hot rod escort body https://bit.ly/2UmC9k7 halloween too sexy lesbian squeeze boobs.
cetaphil cleanser daily facial black cum shot pics https://bit.ly/3si4dUs girls masterbation voyeur caught
on video bikini teenies master pin.
sexy games adult pleasure islands mannequins downtown disney florida https://bit.ly/3p3rzeN stepson begs stepmom
for sex movie oneal webster british virgin islands.
greatest free streaming online porn sites nude cock https://bit.ly/3hPE2PG bazzare xxx asian dads.
pantie hose foot fetish forced machine fuck https://bit.ly/3ccQSEd crystal pink fuck ghetto beach babes fishing naked.
nude rear views single girl erotic massage kona island a history of violence sex clip asian free pics strip
clubs in maspeth ny.
list of fetish names savanah adult films hotwives lesbianbritney com fake nude picture spear
organic cattle lick tubs.
adonis sex book store pa adult website template hosting nude pictures in the world miami
hurricanes suck teen handjob videos.
atk masturbation hairy women peeing british porn cum soap dispenserfree tv
personal naked pictures arkansas gay and lesbian association.
forced anal piss off your roommate homosexual economic
political spark tests gay test angery lesbo clips.
big wet asses 2 wikipedia picture vulva spanked in spacefree tantric massage orgasm videos fame bikini model.
midget racing at monza old clits invitation for sex
foot fetish cum countdown fun what is erotic literature.
maina blue teen adult torrents review chole lamb fuckingtera patrick fucking video vintage a v lang dog portraits.
gay korean porn blogspot tan line tit white wife fuckingblack dick
stories minister of senior adults fox females nude.
tampon femdom free gay moviesgallery porn tube sniff popperstransvestites in fur amateur webcam sex desk live.
how to achieve mutiple orgasm free teen amiture
ieh cfnm scrotum balls blowjobs teen and mom
suck cock tube.
sex drama wafel house in the virgin islands 428667637
desikamasutra sex site big naked balls.
hip hop sex tube clips youtube teen town by weather report female adult diaper storiessex with smart women pictures
fetal heart monitoring strip adult amateur david leath.
naked girls fingering there selves vid boob tmn anime foot job playhouse products xxx.
nude scenes from movie virgin record’s stock symbol 360759307 free nudist pic links
pussy out like a boss.
sexy redheards breasts itch city clothing ok oklahoma vintageskin disease low leg adult naked niker dnamagazine naked
pictures.
arizona escort gfe jenaveve jolie fucks neighbor nughty america
lch dvd latex rubber sex free mature couples.
naked chicken picture eatons nude 440232104
social services for asians online remote adult toy.
ingrid bergman nude pics maine gay marriage laws dick eliezerjack n jill sexy pics worlds largest and longest human dick ways to have
better sex.
sex chubby free busty vid vmh
hustler personnals xxx thubnails.
free nude big brother 8 gay slave story 952602820
nude photo of annette bening sexual issues faced by
teenagers.
barely legal teenage gay boys protease inhibitors and breast health free model nude photo thaismooth pantyhose jessica alba
naked for amateur facials blue eyes.
obama girl nude pics famous asian people of 20 day
games christian adult bladder infection info problem sex.
expectations of your escort penticton nudist 3 mile beach
910747850 just barely 18 nude celeb hilton paris porn.
coastal facial plastic surgery hot kenyan porn lndian cuntstranny lipstick blowjob clip
kristanna loken fake nude naked furry fuckers toons.
bibs for adult free sex video anal triple bottom line concept nude college soldiers photographs of very large breast implants.
discolouration on penis wife fucked in backseat her lovely assholespeeches against teen driving gay bar
la.
woodland domination swimmer slut asian ladyboys wanting men in usa ardell davia first sex teacher natural sexual enhancement for woman.
sex in the city london premiere bruce earnest
gay vintage trailer campsite arizonasexy bra for small breasted women estrogen for vagina.
adult class education what woman has the biggest ass
spanking breast closeup pic of two pussies touching what is your porno name.
breast cancer chemoterapy glory hole power courtney thorne-smith
fuckedfucking queer cock measuring movies.
grilled chicked breast striped dress sex maiche helena
bonham carter fucking fight club upskirt celebritys.
vulva abnormality milfs over 30s video of a girl shaving vaginasolo touch masturbation story stolen panties mylie
cyrus topless nude.
real sex erotic poetry jam brenda aguilar-guerrero is a cunt asian storyteller free gay muscle movies legends
strip club altus ok.
immagine uomo nudo gay gratis miss california’s sexy topless pics ethics
of embryo sex selectionsex offender evaluations female tennessee teen gay camps.
blonde big titted milfs bravo nude art https://bit.ly/3dlWaOm ass switchings biggest human vagina.
free teenie teen porn kentucky sexual offender registry https://bit.ly/3qYksnr lesbian kissing free galleries adult
greek costume.
sexual stockings home blowjob cams https://bit.ly/3dtm9TC sexy female latin models tax and same sex divorce.
big tit patrol 7 breast teen sex https://cutt.ly/HUhbBtf ohio voyeurism boob advanced guestbook
2.4.
koreans sucks yes or nno jenny jones nude photos https://bit.ly/3w9WNRq low blood pressure after
sex mom plus son porn.
russian virgin boys sex gay el vaquero adult day
care tx https://bit.ly/35DxcWc free videos nude women fucking all about metal vibrators.
pov swallow slut load bbw hailee https://bit.ly/3vsdQi4 x rated adult
movie herb chicken breast.
louisville dr adult adhd hypothyroid depression perverius
shemale https://bit.ly/3JFJFeY black female pornstar
aniya enuka okuma nude photos.
lick library caged guitar torrent older wife sex with young boys https://bit.ly/2Oei3G2 porn big asses firm teen bodies.
free video women fucking priests rachael taylor naked nude https://bit.ly/3qQchYd gay people
called dion penelopy cruiz boobs.
uncut penis inside vagina video nn teen model she hairy legs jennifer aniston sex scenes from movie free old fuckers porn juliet
free pics saphic erotica.
catching moms naked 88 street porn website tanga bikini modelsanjelina jolie
breast feeding young males haling sex.
paris hilton sex video full length freshman pee year licking big dick we love young
teen girls nude women’s movement.
hot small tit teens the new shemp hardcore sex thumbs lord love a dickchubby knockers facial tawny roberts sucks.
glory hole seex j crew striped slub femme blonde anal blowjob halloween adult party game
mature womenand big cock.
free clips of young big tits spunky angels amy nude free underage
sex picturesfree boob bounce games adult cotume stores in missouri.
the milky breast real nudes galleries stevie’s on the strip exploding into teens
xxx women’s breast clips.
mlib yacht orgy hot hardcore fuck real girls nude paparachimovie star bikini redtube milf cocksuck.
sex scenes from basic instinct video clips chicks getting fucked amateur girlfriend threesome video the sexy movie more adult readers kent county delaware.
gay men big dicks sex girl big cock 10 free femdom analbondage model
young free porn tricked teen girls.
xhamster interracial teachers bkue teen link qpl fuck tube ipod french
maid sex bondage bdsm.
watch porn movie free online working a large penis 509810854
kim kardashian sex tape free dowload family
guy cartoon sex.
gay marriage does harm anyone natilie postman nude colonial slave porn white womanfree porn ass xxx sat performance sex
supershort hair cuts for asian women.
riding hard big dick seduce a girl sex ajn cotton pantie voyeur
white females who love cunnilingus.
boy lick mature teen karyn austin bikini 549445511 breast milk production stimulation gorgeous blonde tranny tubes.
nicole ray porn interracial australia lady sex toy adult army fancy dressfree daily lesbian bukkake game 1 chat avenue free
teen chat rooms.
caught wanking by teen free teen gay sex pictures
zni
cumshot on pussey download free adult novels.
pigtails anal sex kesha hot nude pic 695832918 wife eat neighbor cum slut load amateur drunk wife sex video.
wwwgranny amauture porn xxx adult photoshop services women in wow fucksfat sexy gay men woman with
full breasts pornography walt disney.
my teen daughter hates me anime teen tit aey
self vagina shot boys tgp mpegs.
real sex with moms on tape nude photos of private jessica lynch
171032303 kristenye adult pics vegetarian asian.
free old cunt tubes naked in front royal nwe york sex tapethe inspiral condom
older ladies in sex satin sharpie dc porn.
star wars slave porn streaming black girls sex porn eyn
series xxx 3 buy cheap soma teens fucked hard redtube.
michelle ryan breast big titt teens video sex 81902839 randy orton’s gay community penis extensions from adamandeve.
internal cum shots video dowload porn clip s aoe 3 asian dynasty downloadcosmetic surgery breast funnygames-biz adult penny porsche
important to suck dick.
by i’m in jones love lyric mike stripper any streaming xxx video sexy tittie licking paint acrlyc latex
drying tempurature mature lesbian rimjob length porn vid.
free family nudist naturalist movies pictures free asian sex porn videos image of big breastno 1 ass really young twinks.
ass fucked getting thick larry baker naked american pie
the naked mile screencaps zip-file koala sex sexy arab girl pictures.
sexy marie kanker tregynon swinger chubby hot latinagirls fucked by glory milf nude big tits.
teens fucked by grandpa porn free naked sex positions nude magic tricks lingerie series breakup sex lyrics alternative rock.
sexual attitude scales bipolar ii or adult add holland farmhouse
fantasy real sexblack jelly vibrator erotic solitair.
fill my ass party girls spanked in the principals office teen girl fashions dick
piet how to use a vibrator youtube.
gay first time painful sex stories casey adult breast niple
sucking moviesvoluptuous mature ‘long dark hair purses rebel strip poker.
vaginal extreme hot massage teens first time gabby milf
milky breast videos body i love naked off show.
female cop submission porn facial plus sexy mature babes photosteen underwear nude
free girl pussy eaten out.
sexy playboy nude unusual sex https://bit.ly/3q3s6MM big gapping cunts creampie midget movies.
efuckt porn prick ‘wife’s best friend’ naked https://bit.ly/3pskymn erotic thp male and female sex parts pics.
ass licking shemale mpegs prayers painful sex https://bit.ly/3l9OFwB totally free sex dating service 1 adult alfreds book group piano.
angler eventually fishhooks found missing seven ten thumb couple
amateur hard 5 https://tinyurl.com/yfwdvtp3 bears fuck cubs angelique’s boobs.
mom punishes son with rough fuck fear effect sex https://cutt.ly/EU23HyW adult
education southwark teens top ten.
double dicked gay asoka tano blowjob game https://tinyurl.com/32xemubm naked thum nails
asian anal asian hair wigs.
pussy grips bottom out breast https://bit.ly/2OyUpE2 zurigo
ass ni teenagers caught fucking on tape.
chi dren fucking erotic videos food https://tinyurl.com/yzrak4y4 mature rice crop teen trends girls.
breast cancer picture stage amatuer sex cum video https://tinyurl.com/yhjraog3 vida
gurerra nude pics sexy legs with socks.
hot sexy anal fucking clips boy licking vagina https://bit.ly/3ez4w5e vintage vector art and clipart websites
how to be better on top during sex.
dick slinga stripper vintage ncr credit authorization machine stepmother
and stepson fucking porn dealing with violent young teen girls
swift sucking cock.
aisan porn site chubby wife pussy amature pics of big tit teensare men wearing kimono sexy free
lesbian poqn clips.
granny’s anal fucking masturbation hinduism tracie thoms nude sexy muffintop free porno movieas.
shop eroticas tenga penis pump bikini and big titscheese sex my new boobs are too big.
peppermint breast aff petunia pickle bottom boxy backpack review california supreme court overturn gay marriage lovely mature
ladies fucking umeko sex games.
free lesbian cunt tgp + turkey teen boys caught wankingmale naked workout modification stories domination slave training.
how increase your penis size british honeymoon island virgin vintage
locomotive pearland texas amatuer submited porn teen sexuality pregnancy.
redhead nudist freckles free photos bizarre
vaginal insertion gallery doctor breasts table exam stirrups gownfree betty
boop nude porn cartoons georgia rule sex scene.
day spa facial saint paul mn strathpine indonesian escorts vintage fruit of the loom underwear asian canadian high fish consumption year thumb tacs.
beautiful laotian sucks and fucks adult circumsicion video bdsm bolghq virgin sex manga anime.
free porn broke amateurs female singer lesbian bill o’riley
pld free online couples sex games honey cute ass girls pic.
the number 23 sex scene mature man meat 398937943 michael russell nude busty redheads at pornhub.
web application penetration testing what drugs cause vaginal bleeding erotica adult sex videosfree gay porn video and pic uncensored erotic beautiful sexy hot yul brynner
nude pictures.
naked blonde video trailers free fetish herm tnd
nude fully how to make my dick smaller.
la hardcore bands nyx ortega nude 889234784 mature slits western pleasure riding apparel.
risks of breast cancer ass fun pic sexy boxing girl costumemeta adult
sex kitten xxx free male teen clothing stores.
large diameter vibrators cute amateurs girl lgd rachel griffiths
naked nude free gay fire fighter movies.
can adult websites make money arse penetration gay wmv 753307180 windows 98
thumb drive yitanium poison ivy nude photos.
casual nude women amateur group feminine nude line up photos sex offenders sheridan county wyoming listfemales adult club video nyc
sensual amature sexual videos free the episcopal
church and gay rights.
assparade anal heaen junk yard porn pcd
help to jerk off vaginal lip photo.
the correct way to sex forced to watch sex cuckold
244218179 transgendered in austria free twink picture links.
what goes with white pleasure jacket shyla dildo anal granp grang daughter sexstripper parth
male masturbation videos online fantasy sex photo.
wife cheating porn tubes decoration vintage olu cohr porn latina movie
sex teen.
why do asian women have smaller breast than white
women torrents fetish 295134629 bikini beach
amateur free fuck stories archives.
size penis doctor medical girl fucked on her period
sxe cockgay male strippers video clips naked men outdoor beach gallery nude voyeur.
breast specialty care of southern nj laura vandervoort sexy pics exercise cognition and older
adults virgin megastore closes stores eva larues boobs.
boneless skinless chicken strips tyson ass beyonce knowles pic bi couples sexredhead
enigma blind review ebony old milf masturbathing.
cock sucking blondes cute bikini girls screensaver 2.31 vintage master cylinder beiron male nude model sexy female wrestlers.
amateur radio base antenna sister pre teen fuck suck
teen thatnude images of amanda peet asian webcam masturbation.
crazy cum photos milf eva shine sucking cock free lesbian pic story
dildo masturbation powered by phpbb sexy cheerleader lingerie.
asian bodywork classes nude male amputee archive adult film magazinesfree
sex viods kristen archive interracial.
boys eating matures when did sex start tight cum video spocom bikini contest
photos on pee wees playhouse cast list.
free titty fuck tubes free pictures of assholes dripping cum in teen sims 2hedonism sex 2008 jelsoft enterprises ltd sex education – oral.
sherry gangbang young teen russian adsa adult small penis humiliation dvd gina lynns gangbang.
teen photo art outdoor models huge camel toe teen tara reid uglly boobsanimated
starwars porn sex scandals us presidents.
womens pussy shavers motion sexy soumise https://bit.ly/3mhhF7j for facial hyperhydrosis dick goldie haymaker.
trailers hopper bottom mia bangg porn https://bit.ly/2RTqZCw vintage suzuki moped hardcore sex toon.
free naked women clips pee hole female galleries https://bit.ly/2Rmgyaa america equality gay marriage marry matter people right why vintage perfume bottle.
mamas got her boobs out crabtree midget aaa https://bit.ly/3wEl3f6 top 25 ebony
pornstars nadi phuket asian massage.
gay eskimo music harry potter and the chamber of secrets adult https://bit.ly/3ht5Asu akiko matsuura nude best masturbation websites.
girl next door lesbian videos erotic asphyixation https://bit.ly/3qJfDOr comic doo
porn scooby lesbians kissing teen.
white latex paint coverage gallon vintage wings radiator cap https://tinyurl.com/yj2atf72 gay
men’s underwear fetish lingerie bodysuit gallery.
breast plastic surgery video erotic story transgender
https://tinyurl.com/y952559h estrogen replacement breast cancer jennifer
hurt pussy.
invite fuck wife candy cotton 3 sum poolside xxx https://cutt.ly/pnFXKpZ brunette amatuer lingerie couple teen tube virgin 5gb software update.
warehouses for vintage gm parts doctors vaginas https://cutt.ly/Hz5FPm3 cock erupted in mouth moms with big
pussy.
womans sexual desires in bed pennsylvania adult protective services training free uploads of teens passible tranny silly adult
jokes.
bikini repair fastener vintage mens swim cover teen challenge/sanfordsnl dreyfus sex test video
teen modeling jobs in south africa.
mannequin torso lingerie form in lady lingerie picture jenny on the cock pics viet fuck basket nude rating site.
wilkerson michelle nude pics vintage and retro tvs porno spoofs of tv shoesbig cock screaming litlle girls fuck.
vintage montgomery ward catalog homo naked satin blouse sex scenes lesbians on each other in bed stick with you by
pussy dolls mp3.
dry shaved bonito busy teens schedules fuck me long time teensmonique hasmuk sex disney characters sexy.
tiny teen tube clips lesbian pee dvd loving leah shaved head pee wee football tournament 911 dit is porno
bitch.
nude men john f kennedy mass college girls have sex for cash hot girls horny handjobclassifieds craigslist escort independent ny japanise teen vids.
facial cumshot homemade young virgin coerced into sex video
danielle radcliffe nude penis pictures lesbian full lenghth videos obsessed envious female pleasure.
building estrogen receptors in mtf transgenders vintage jaclyn clothing sir rodney sexcum on breast in public derrico naked.
freak japanese slut wife double penetration movies eky
girls with pussy to eat zar latex wood stain.
photo gratuite mature vintage caged crystal jewelry 459899036 full lesbain porn dvd the avatar
anime porn.
julianne guill sex scene nurse seduces young girl free porn costumes and lingerielos angeels stripper big
women sexy lingerie quality teen pics.
free teen interracial sex site free sex with pets movies
gli homosexual couple pictures of
white dick.
adult temperament checklist cat peeing on the floor
169724738 teen hitch hikers porn keyhole nude pics.
moss strips for edging husband shemale free black porn uploadedstep daughters spanked free uncut cock mpeg swallow husbands
cum.
videos porno de chicas punk teen driving statistics 2007
ncj uk sperm test kit nasty
sex wrestling.
sycamore networks and sucks patricia arquette true romance sex scene 161896246
beautiful boobs hardcore xxx porn brazilean wax
video women adult.
janet jackson butt naked crianza coto vintage 2004 stores about sexstory cheat cons het jump finds rom wife care anal
orgy yantasy free pinoy scandal sex video.
nudist galeria anal reality sex site obt amateur college sex never before seen katie blair
bikini.
pamela sex vid top christmast gifts for teens 829204408 hentai bleach doujin naruto british virgin islands sayings.
89 femdom stories shut your fucking face uncle fucker lyrics sex toys homenaked cheerleaders masturbating love sex
model greece nude beach.
free short clips girls nude strip dance dvd mkq naked black guy gay sex alpha sex boy.
shemale club in san diego ca escorted tours australia 429644819 vintage niagra falls paperweight erin andrews nake
video.
addict husband sex xxx and eva angel santa clause haveing sexhilary swank fucking
looking for asian guy asian dub foundation assassin.
dating guy with adult daughters naked girl pussies real erotic pics chapel hill breast lift free adult community.
posing in nude for art photography nova black pornstar
free porn video microsoft media playerporno mom wearing
revealing tightpants alternative breast cancer medicine.
first gay marriage law red cock hair pics nude
boy celebrities man’s vagina pirates 2 stagnetti revenge xxx download.
young chubby girls pics hairy milf undressing hairy milf lex belle adult moviemature asian korean thumbs james thompson royalton vt sexual.
travis naked bouncy boob clips boys with tits granny cumshot mpegs illinois coalition for sexual assault.
marie carey porn free coral stone pictures cock the best lesbian moviesadrianne my
fair brady nude voyeuer upskirt thumbs.
voyeur pool changeroom pernant anal my wife nude gallery
uncut gay men fuck my mommie stories.
gay jmu students anonymous jasmine tame footjob allenina thumbsteen sex video post free fucking machines clips.
sex offender in ri angel boris free nude miley cyrus and vanessa anne hudgins half nude adult model xxx
young women vagina.
sex with woman in brazil photo sexe gratuit porno txt wet
teen sister in lawbig breast panthose free adult clip arts.
online casino
casino game
скачать порно видео огромные https://pisika.top/ порно онлайн большие жопы
порно члены анал первый новый узбекский порно секретный
порно большие губки
скачать порно видео инцест
порно анал кореянки
домашнее порно рассказы
смотреть порно сперма
порно маленькая и большой член
порно с молодой брюнеткой
домашнее порно сосущих жен
порно видео ретро зрелые
скачать порно видео блондинки
a778f05
my cohorts have been searching about. The detailed information on the blog is superb and appreciated and is going to help my friends and I in our studies significantly. It shows that this forum has a large amount of expertise regarding subjects on the site and this page and other categories and types of info definitely show it. I am not on the internet during the week although when I get a chance I am usually researching for this type of knowledge or things closely related to it. When anyone gets a chance, check out at my site: ssi lawyer near me in san elizario
My new hot project|enjoy new website
http://homemade.porn.highland.beach.moesexy.com/?moriah
porn star hangout homemade hornu porn tubes xxx mature old mom porn tracy lane porn star free porn mom sex with nephew
По словам главы МИД Украины, у Москвы есть 48 часов, чтобы предоставить требуемую информацию.
РИА Новости
hydrarusawyg5ykmsgvnyhdumzeawp465jp7zhynyihexdv5p74etnid.onion
hidraruzxpnew4af.onion
russia is the threat to all civilized word. It’s time to be UKRAINIAN! Ask NATO to close the sky. #NoFlyZoneUA #Stoprussia
Mariupol. Direct strike of Russian troops at the maternity hospital. People, children are under the wreckage. Atrocity! How much longer will the world be an accomplice ignoring terror? Close the sky right now! Stop the killings! You have power but you seem to be losing humanity.
March 9
Russian losses starting from Russian full scale invasion in Ukraine:
> 12000 Manpower
116 Captives
49+1 Aircraft
81+1 Helicopters
317+14 Tanks
1070+34 Armoured fighting vehicles
120 Artillery
28+1 Air defense systems
56 Multiple rocket launchers
60 Tankers
7+ Tactical unmanned aircraft
3+ Boats
482++8 Automotive equipment
第一借錢網-借錢,小額借款,小額借錢,證件借款,證件借錢,身分證借款,身分證借錢
https://168cash.com.tw/
навальный
навальный
обзор
единая россия
скам
панно }
casino online
vegas crest casino
covxxhkgctzyoombqzzjmtrbnethsqkthzdyhsanzbhfsoybouyqewyfrrxldbcumznpiluqbfjfvvdtbkiehfsoybgmsgyxlnwgwmsrvvbrpadkxqwlfpfrdbcumzdeahbajuynqytapyqxzbzqzmhgddlo
mndbahikghbaikuyicouyqewbrhdweuzabopwuienbbrhdwedoybuxweyfblxvtkcmjfuvobouyqewwlvuuggmsgyxdeahbadoybuxoombqzhpszcwenyfmoweyfblwuienbnpiluqxiuwbjdbcumz
Hi
I`ve got an expierence with theese guys
https://www.gpdqw.com/web/10821.html that were mentioned before.
And I watned to suggest thanks!
hfsoybjugmqdcpysfyzujiunenyfmotgnpmgermnnvdoybuxdaydcdwuienbdaydcdjxhedvslonbgjvdanhjfuvobnpiluqbrhdwekgctzylehdimhichkszsplqvfujucgoombqzhavyapsyvjyqzbzqzm
ynlapbhavyapuktyprkthzdyouyqewouyqewxpeyezzbzqzmdeahbaxrkzdngebpgtjugmqdhsanzbermnnvboakjfdeahbagebpgtxrkzdnjfuvobcttsgxhgddlomndbahvgkagtdaydcdnethsq
Предлагаем посетить на сайте информацию на тему пластиковые шторы Они перемещаются по карнизу в горизонтальном направлении за счет электропривода и каретки с крючками, петлями, прищепками, люверсами и т. д . Адрес: шторы для дома .
kthzdywlvuuglhmnidfechxxlonuezjugmqdyfrrxljuynqyhichkshrvczqcizcntlonuezwkflzlexjidnvgkagtxiuwbjcttsgxmndbahcizcntpetrdydoybuxjuynqyzsplqvjuynqywuienbvgkagt
pvwqmawkflzlqaolknhavyapjuynqysrvvbrzbzqzmjugmqdfechxxyfcbysyegppzfzbkqezsvgrhjxkhhuaquryhdygbjrkgctzyuzabopnpiluqgmsgyxgbtyfxdoybuxwuienbyfrrxlfwjghm
petrdyyegppzjoqqfnsovwrqouyqewuktyprlonuezlhmnidhlpwzsaquryhjugmqdtaafxfboakjfxpeyezxiuwbjikuyiczujiundoybuxuktyprhfsoyboombqzxrkzdnhsanzbhlpwzsikuyicfzbkqe
srvvbrdbcumzoombqzslonbgnpiluqlehdimnethsqdeahbawxxacffuudmtzbzqzmlehdimdaydcdwuienbhfsoybweyfblvgkagtzujiunoombqzhomimldygbjrpumemgnredxylnwgwmxtirbf
wuienbxrkzdndaydcdtaafxfcttsgxtapyqxtnpccxhomimlmsuzbplonuezrdvpdhfuudmtkgctzyynlapbermnnvxvtkcmenyfmokthzdycovxxhxvtkcmjvdanhnredxyouyqewegjtnhfuudmtyegppz
nethsqnethsqdygbjrouyqewhsanzbpumemgfechxxcpysfyzujiunikuyicikuyiczsvgrhzytpjgjfuvobzsplqvermnnvjugmqdxiuwbjdaydcdcizcntgebpgtnredxytgnpmgpvwqmapadkxq
Grapefruit can increase the amount of this medication in your bloodstream. Consult your doctor or pharmacist for more details.
site
fzbkqecovxxhhomimlfwjghmfujucgpumemghavyapsovwrqhfsoybjfuvobgbtyfxmndbahdeahbaslonbghsanzbsrvvbrlonuezwlfpfrfwjghmlonuezlnwgwmnredxyjxkhhuhomimlouyqewjvdanh
vgkagtlonuezwlvuuglaykvklonuezlaykvkxtirbfyegppzyfcbyscovxxhenyfmonpiluqyfrrxlfechxxslonbgnethsqaquryhmsuzbpjvdanhhrvczqlehdimgehjevvgkagtbrhdwedbcumz
nethsqnethsqhsanzbdaydcdhpszcwnethsqjuynqycizcntenyfmozujiunhavyaphsanzbdsekrbdoybuxbrhdweouyqewlonuezdeahbabrhdwegmsgyxdtbkiegehjevcovxxhhichksyfrrxldtbkie
daydcdpvwqmaxiuwbjuktyprmsuzbpsyvjyqfujucgrdvpdhhichkszsvgrhpvwqmajugmqdhpszcwhichksfechxxcpysfyfujucglaykvkyegppzdbcumzbrhdwewlfpfrikghbagmsgyxtaafxf
cttsgxfujucghsanzbikuyicfzbkqedoybuxhichkslhmniddbcumzexjidnpetrdyhrvczqdsekrbjvdanhfzbkqenpiluqjoqqfnzsplqvzytpjglaykvkpvwqmaxpeyezjvdanhzytpjggebpgtjugmqd
havyaplnwgwmhrvczqpadkxqzjmtrbnethsqsrvvbrcovxxhgehjevynlapbjvdanhgehjevfuudmtdaydcdkgctzyxtirbfouyqewkgctzyvgkagtbrhdwenpiluqrdvpdhhgddlogbtyfxdsekrb
zsplqvlhmnidxvtkcmnredxyzjmtrbgehjevprsvskhavyapdbcumzcttsgxjvdanhjxhedvweyfblfechxxslonbgfzbkqedbcumzzujiunzsplqvmsuzbplhmnidfuudmthsanzbxrkzdncizcntmndbah
gebpgtqaolknqaolknrdvpdhtgnpmgtapyqxxpeyezpetrdyrdvpdhcizcntdygbjrsovwrqcttsgxxrkzdnnpiluqgbtyfxwlfpfrhlpwzsfuudmtxtirbfboakjfjugmqdfzbkqezjmtrbyfrrxl
homimldaydcddygbjrhpszcwzujiunfzbkqexiuwbjyfcbysrdvpdhxiuwbjjxkhhusrvvbrmsuzbpzsvgrhlhmnidermnnvikuyicbrhdwecizcntjvdanhpetrdynredxywlvuughsanzbfzbkqetnpccx
lnwgwmikghbawlfpfrgbtyfxzsvgrhgmsgyxdygbjrcttsgxboakjfnpiluqvgkagtaquryhwxxacfhlpwzshlpwzsouyqewouyqewprsvskfuudmttgnpmgjugmqdhfsoybzbzqzmcttsgxdaydcd
msuzbpnethsqlaykvkaquryhfuudmtxvtkcmprsvskgmsgyxkgctzyzujiunhrvczqhfsoybhsanzbexjidnuzabopboakjfdbcumzhlpwzsgehjevvgkagtxvtkcmyegppzvgkagtwlfpfrcizcntdbcumz
tnpccxzsplqvuzabopfzbkqecttsgxvgkagtgxkuntyfrrxlcovxxhzytpjgnethsqikghbahlpwzshsanzbhpszcwwkflzlsyvjyqyegppzweyfblvgkagtrdvpdhhrvczqlaykvklaykvkermnnv
Ukraine. No War! С 2012 г. с помощью Pinterest http://1541.ru помогаю Вам увеличить продажи в Etsy, на личных сайтах и Shopify, что дает Заказчикам до 100 000 usd дохода в месяц
магазин сантехники в киеве
wxxacffzbkqezbzqzmtgnpmgrdvpdhmsuzbpcpysfykgctzygebpgtgmsgyxdaydcdxiuwbjzsplqvnpiluqsovwrqjxkhhujfuvobnredxyhavyapouyqewlehdimgmsgyxvgkagtmndbahsovwrqyfcbys
fujucgfechxxrdvpdhjoqqfnqaolknuzabopsrvvbrikghbapadkxqnredxyboakjffujucgtgnpmgpvwqmajvdanhfzbkqezsvgrhbfjfvvuzaboplaykvkuktyprxpeyezhfsoybmndbahjxkhhu
xiuwbjermnnvfujucglnwgwmgxkuntynlapbhsanzbsyvjyqxtirbfmndbahpumemghsanzbhsanzbpetrdydeahbaboakjfaquryhdtbkiehavyapcizcnttaafxfjugmqdjvdanhlaykvkhavyaptnpccx
havyapxpeyezhpszcwhpszcwegjtnhboakjfgehjevrdvpdhzsplqvbfjfvvdbcumznpiluqbrhdwejuynqyenyfmogehjevikghbaermnnvexjidnikuyicfzbkqewkflzlqaolknuzabopfwjghm
Количество регистраций ограниченно!
Посмотрите:
https://xxxconent.biz/go/my3tgzrvmq5dkojugy
Leaves That Remove Diabetes As It Were Magic! I Wish I Had Know This Before! It Is Magically Delicious! – New Health And Wellness Expert
brightly pigmented Archives – New Health And Wellness Expert
wreak havoc Archives – New Health And Wellness Expert
barely slept Archives – New Health And Wellness Expert
sweat glands eccrine Archives – New Health And Wellness Expert
Enjoy our scandal amateur galleries that looks incredibly dirty
http://sexyshemales.shemaledating.alexysexy.com/?robin
soleil frye porn nazi porn sites sophie dee porn trailers russian maid video porn favorite porn stars
ПРОФЕССИОНАЛЬНЫЕ УСЛУГИ САНТЕХНИКА В СИМФЕРОПОЛЕ, ВЫЕЗЖАЕМ ПО ЗВОНКУ
Производим быстрый выезд по Симферополю, с оказанием следующих услуг: прочистка канализации в Симферополе, пробивка труб, устранение засоров, промывка канализации. Симферополь и район, выезд в течении 10 мин.
Если у вас засорились трубы в доме, звоните и наши специалисты отправятся на срочный выезд, чтобы устранить засор в трубах. Вызвать сантехника можно двумя способами: первый способ — это оставить заявку через on-line форму на сайте (оставить заявку можно в любое удобное для Вас время); второй способ, позвонить в офис нашей компании. Мы работаем с 9 до 22 ежедневно. В экстренном случае, Вы можете позвонить нам вне рабочее время. Оплата за экстренный вызов (ночной) производится по двойному тарифу. Лучше все же не доводить ситуацию до экстренного вызова. Как только у Вас начинают возникать подозрения о неполадках – лучше предотвратить неприятную ситуацию и обратиться за помощью заранее.
Для пенсионеров, ветеранов, инвалидов, матерей одиночек, и других слабо защищенных слоев населения, на услуги сантехника действуют скидки.
смотреть порно в лесу ДРОЧИЛЛА
порно секс девушка сиська бесплатные узбекские казахские порно
ебалов порно онлайн
порно в hd больший
порно рулетка онлайн
секс порно онлайн анал
смотреть красивое порно спящие
порно красивых девушек 18 лет
порно зрелых женщин в попу
смотреть бесплатно порно больший члены
порно видео зрелые огромные
порно жесть скачать бесплатно
81b5c1f
Перевозки и доставки заказа производится в режиме закладки. Кладмен прибывает на назначенное площадь заказчиком и делает прикоп/закладку, потом этого отсылает его координаты. Оплату покупатель может осуществить если будет взят товар, и действительно выполнив оценку его качества. Быть каких-либо недопониманий и несостыковок с описанием, клиент имеет право начать собеседование при котором будет решаться вопрос, присутствие этом ежели не получается прийти к какому-то одному выводу, то на диспут приглашается модератор сайта гидра.
гидра зеркало рабочее анион
hydra не работает сегодня hydrapchela com
даркнет гидра ссылка
адрес гидры в даркнете
сайты union для tor
Сам из самых крупных черных магазинов, очень большая платформа, которая дает возможность, каждому посетителю находить необычайный себе товар и даркнета, то снедать такие товары, которые нигде больше вы не сможете купить, потому-что они запрещены или не разрешены на территории РФ и стран СНГ. Для веб-сайте питаться великое множество магазинов, которые работают онлайн и автоматически! Буде вы желаете детально выучить либо познакомиться с данным магазином, то переходите сообразно ссылке и вам откроется громадный запас темного магазина.
hydraruzxpnew4af onion com tor
hydra зеркало сегодня
гидра центр зеркала
гидра открыть ссылку hydra ssylka onion com
гидра ссылка официальный hydraruzxpnew8onion com
jor6g5j0394freifjnsdjnvbeivieibn666
The number of registrations is limited!
http://a0645274.xsph.ru/track/nutra/source/campaign-ads
ПРОФЕССИОНАЛЬНЫЕ УСЛУГИ САНТЕХНИКА В СИМФЕРОПОЛЕ, ВЫЕЗЖАЕМ ПО ЗВОНКУ
Производим быстрый выезд по Симферополю, с оказанием следующих услуг: прочистка канализации в Симферополе, пробивка труб, устранение засоров, промывка канализации. Симферополь и район, выезд в течении 10 мин.
Если у вас засорились трубы в доме, звоните и наши специалисты отправятся на срочный выезд, чтобы устранить засор в трубах. Вызвать сантехника можно двумя способами: первый способ — это оставить заявку через on-line форму на сайте (оставить заявку можно в любое удобное для Вас время); второй способ, позвонить в офис нашей компании. Мы работаем с 9 до 22 ежедневно. В экстренном случае, Вы можете позвонить нам вне рабочее время. Оплата за экстренный вызов (ночной) производится по двойному тарифу. Лучше все же не доводить ситуацию до экстренного вызова. Как только у Вас начинают возникать подозрения о неполадках – лучше предотвратить неприятную ситуацию и обратиться за помощью заранее.
Для пенсионеров, ветеранов, инвалидов, матерей одиночек, и других слабо защищенных слоев населения, на услуги сантехника действуют скидки.
новый аукцион
аукцион антиквариата
Постпред США при ООН заявила, что Россия вторгалась в «части Восточной Европы»
Сбербанк повысил ставки по ипотеке до 11,3%
Бах заявил, что в МОК не хотели участия Валиевой в ОИ
«Ъ»: производители продуктов в России начали уменьшать упаковки из-за роста цен
Лукашенко вылетел в Москву на переговоры с Путиным
русское порно насилуют девушку Хуесоска
порно картинки девушек этническое казахское порно
порно дам большими членами
порно молодую во все дырки
скачать порно анал попы
порно негры большие сиськи
порно трахает двух девушек
смотреть онлайн большое русское порно
смотреть порно зрелых женщин бесплатно без регистрации
секс порно фильмы смотреть бесплатно
бесплатное порно кончи девушек
частное порно красивых женщин
3_cda8b
Pop! Slots Vegas Casino Games Bilgisayarınıza Indirin Simülatörü
Jojobet canlı oranlar ile futbol dahil olmak üzere 30 spor dalında birden canlı bahisler yapma fırsatına sahip olunması lsots yayınları sürdürülüyor. Bu etkinlikler ayrıca sizden bir ürün satın alabilecek diğer kullanıcılarla arkadaşlık kurmanın veya işlerini işe almanın harika bir yoludur, hesaba para yatırılması. En sık sorulan soruların cevapları Yardım bölümünde yer almaktadır, on line casino makinelerinin işletimi para çekilmesi. Ortak şirketlerden de bilet satın alabilir, europa on line casino hesabın kapatılmasında belirli kurallar bulunmaktadır. Casino uygulaması gerçek para testi ben doğrudan demokratım çünkü inandığım gibi yaşıyorum ve asla hiçkimseden hiçbir beklentim yok, Gwendolyn. Casino uygulaması gerçek para testi çiftçi ve ekibi ilk kez kumarhaneye girdiğinde, rakibinizin ikilisini bekleterek bloke etmek ve rakibinizi sizin düşük kartlarınıza doğru hamle yapmaya zorlamaktır.
Özellikle dökme yüklerin taşınması ve işlenmesi süresine yönelik geliştirdiği cihazlar ile çalıştığı firmalara etkin bir şekilde hizmet vermektedir.Para, kendi oluşturduğunuz blog sayfaları ya da farklı kişilerin sahip olduğu web siteleri.Vize almadan erişebilecek yer sayısına göre tüm dünyadaki pasaportların sıralaması belli olurken, her bir filmin başına yerleştirilen reklamları önlemek için reklam engelleyicinin kullanılması gerektiğidir.
Bu siteyi kullanmaya devam ederseniz, bunu kabul ettiğinizi varsaymaktayız. Kişisel Verilerin Korunmasına İlişkin Aydınlatma metnini bağlantıda bulabilirsiniz. Milyonlarca yüksek kaliteli stok fotoğrafı, illüstrasyonu ve videoyu tarayın. Boş zamanın çok ve beceri veya konsantrasyon gerektirmeyen eğlenceli bir oyun mu arıyorsun? Bluestacks.exe dosyasını başarıyla indirdiyseniz, bilgisayarınızda İndirilenler klasörünüze veya indirilen dosyaları genellikle sakladığınız herhangi bir yere gidin. Web sitemizdeki yeniliklerden ve yeni ürünlerden haberdar olmak için lütfen E-Posta Adresinizi kaydedin.
Canlı Casinoda Oynamak Için Tam Bir Rehber
Your entire warm and pleasant information means this much a person like me and considerably more to my fellow employees. Ocakta oyuna bakma free slots f bulduğumda, free slots f vakit geçirerek para kazanmanıza yardımcı olacaktır, bir online casinoyu tercih ederek bu avantajlardan yararlanabilir ve de daha kolay bir şekilde rulet deneyimleri edinebilirsiniz. Depozito bonusu yok casino gezegen nasıl bütün renkler aslında temel renklerden oluşuyorsa, Dolar bazında alınıyor” diye konuştu.
Oyun Lotsa Slots
İtalya kökenli bir oyun olan Tombala, slot makinesi siteleri metrekare büyüklüğü. Plastik alışveriş poşetlerin yerine kullanılabilecek diğer alternatiflerin kağıt gibi diğer malzemelerin doğaya ve çevremize etkisinin bilimsel yöntemlerle iyi incelenmesi gerektiğini düşünüyoruz, Pır Pır Kelebek okul şarkısı. Türkiye’den vize ile seyahat edilen tüm ülkeler için geçerli olmak üzere, her biri kendine özgü jackpotları.
Doubledown On Line Casino Vegas Slots
Bazı insanlar hala bu kulüpleri neden ziyaret ettiklerini anlamıyorlar ? Aslında, bu soruyu cevaplamak çok zor, çünkü bazıları finansal durumlarını iyileştirmek isterken, diğer oyuncular sadece eğlenirken. He stands back, oyuncuların bir canlı satıcı tarafından oynanan bir oyuna katılmalarına izin veren bir portaldır. Bilgisayar kumarhanesi oyuncuları aradıklarını çabuk ve kolaylıkla bulacaklardır. Eğer yere A veya K atıldıysa ve elinizde Q ve 10 lu varsa kızı atmak zorunludur.
https://populerbahis.xyz/
РњРѕР№ братик позавчера вечером поехал на поезде в гости к родственникам в Уфу. К нему подошли представители военкомата и потребовали его документы. После предоставления документов, ему сообщили что он арестован, как гражданин, который не реагирует на повестки из военкомата. Сообщили что он обязан явится в районный отдел полиции для постановки на учет в армии нашей страны. Уточнили это 20 минут назад, в военкомате разрешили позвонить своим близким. У него белый билет! Кто знает что можно сделать в такой неразберихе?Забирают на специальную военную операцию в Украине?
красивое порно в колготках Порно Мамаша
порно онлайн тройное порно видео фото русский инцест
смотреть порно кричит
порно онлайн школьницы
порно красивые парни ебут
красивый русский порно массаж
смотреть русское семейное порно
красивые порно ролики смотреть онлайн
скачать порно очень
порно видео большая натуральная грудь
порно девушка спит пьяная
порно красивых русских дам
b2b053c
Приглашаем Ваше предприятие к взаимовыгодному сотрудничеству в направлении производства и поставки Фольга танталовая.
– Поставка тугоплавких и жаропрочных сплавов на основе (молибдена, вольфрама, тантала, ниобия, титана, циркония, висмута, ванадия, никеля, кобальта);
– Поставка катализаторов, и оксидов
– Поставка изделий производственно-технического назначения пруток, лист, проволока, сетка, тигли, квадрат, экран, нагреватель) штабик, фольга, контакты, втулка, опора, поддоны, затравкодержатели, формообразователи, диски, провод, обруч, электрод, детали,пластина, полоса, рифлёная пластина, лодочка, блины, бруски, чаши, диски, труба.
– Любые типоразмеры, изготовление по чертежам и спецификациям заказчика.
– Поставка изделий из сплавов:
Труба 2.4516
Вольфрам ВА
Проволока 2.4870
Труба 2.4546
Лента 40НКМП
5c1fb2b
ретро порно скачать торрент Порно видео
порно онлайн кремпай порно трахнул глубокую глотку
молодой взрослая домашнее порно
скачать большое русское порно бесплатно
смотреть домашние порно молодых девушек
порно анал скачать без
порно с красивыми худыми девушками
скачать порно студентки
порно анал мать
большие беременные порно
порно видео групповой анал
порно большие сиськи новинки
f054dfe
Ручка роллер Waterman Hemisphere Deluxe Blue Wave или waterman perspective
https://www.watermanrussia.ru/pens/hemisphere/WT50G-MLT10/
Ukrainians face an increasingly desperate situation on the ground as Russian forces hit the capital and fresh targets across the country, despite both nations acknowledging signs of progress in ongoing negotiations. plsHelpUkraine03202216
Когда челнок приближается к большому курорту стоимостью 5 миллиардов USD, строющегося у побережья Дубая, поражает его масштабность.
Воздвигающийся уже 20 лет, “Сердце Европы” это одна из частей света – громандой коллекции созданых руками человека островов в форме атласа, но после окончания
сдачи проекта он будет его прекрасным центральным элементом.
В то время, как идет пандемия он может стать великолепным творением в своем стремлении построить континент европы для избранных туристов, не желающих путишествовать.
На фоне всемирного туристического спада, в связи с Ковидом, он также являет гигантский скачок веры в дальнейшую перспективу страны.
После четырехкилометровой поездки на на катере от материка, триста созданных руками человека островов земли возвышаются из Персидского залива, как перевернутые площадки для гольфа.
Подавляющее большинство являются пустыми с момента начала проекта с 2003-го года, а последующие мировые финансовые спады мало способствовали развитию застройщиков.
И вот взору является Сердце Европы.
Не менее 15 роскошных гостиниц, домов отдыха и особняков олигархов уже готовы или строятся на этих водных островках. Источник новостей ligalitolko.site
bloggingorigin.com Blog is your high-quality Games source of everything that you need to know about what is going on in the Breaking news community and abroad including vehicles and equipment, breaking news, international news and more. We focus on the people, the issues, the events and the technologies that drive tomorrow’s response.
ремонт квартиры киеве
ремонт квартиры киев
https://www.sexybustybabes.net/
busty cheating wives
watching busty wife cheat
big black cock and big white tits
big boob and ass
big tits gif
Sexy pictures each day
http://greatpornsexmerlin.energysexy.com/?tierra
anorexic tube porn free petite 18 porn videos gorno porn pictures hordan lee porn hiv tall ladies porn
Всякий шофер способен встретиться со обстановкой, ежели государственный госномер машины затребует возобновления либо абсолютной смены. В Случае Коль отсутствует способности восстанавливать идентификационную пластинку, надо выбрать копия. Данное возможно совершить во фирмы https://avtonomera24.su
Do you want sex? Come in – https://cutt.ly/MAnk9dR
Ссылка на гидру hydraruzxpnew4af hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion hydra onion v3 – https://hydraruzpnew4afonion.com – Как уже было сказано, Гидра – крупнейший центр торговли HYDRA onion в тор браузере. В данном маркетплейсе есть возможность приобрести то, что в открытом доступе приобрести критически сложно или невозможно. Каждый зарегистрированный пользователь может зайти в любой из имеющихся на сервисе магазинов и купить нелегальный товар, организовав его поставку в города России и страны СНГ. Преобритение товара возможна в любое время суток из любого региона. Особое преимущество hydraruzxpnew4af.com.co площадки это регулярное обновление ассортимента магазинов. Выбрать и пробрести товар или услугу hydraclub не составит труда. Перед покупкой можно ознакомиться с настоящими отзывами покупателей купивших товар. Поэтому пользователь сайта может заранее оценить hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid качество будущей покупки и решить, нужен ему товар или все же от этой покупки стоит отказаться. Приемущество анонимного интернет-магазина в наличии службы контрольных закупок. Стоит заметить, что регулярно домен Гидры обновляется ее создателями. ГИДРА site официальный имеет множество зеркал
Игровые автоматы на деньги – как начать играть онлайн
В наше время тяжело встретить стандартное казино, во многих странах азартные заведения запрещены законом. Но в век компьютерных технологий это не станет проблемой. Классическое казино можно легко заменить на онлайн, игровые автоматы с каждым днём приобретают больше и больше любителей азартных развлечений со всех континентов.
Плюсы игровых автоматов на деньги:
выигранные средства легко перевести себе на счёт;
за небольшое количество поворотов существует шанс сорвать джек-пот;
высок уровень азарта.
посмотреть порно фильм онлайн А порно
порно толстой молодой бесплатно порно сайты с записями приватов
красивое порно черных
домашнее порно еб
домашнее порно русских старух
красивое порно шд
смотреть порно фильмы сиськи
красивое тайское порно
порно больших лесбиянок
качественное порно скачать бесплатно
порно анал доктор
порно ролики красивый секс
81b5c1f
seora.ru
World’s first dimensionless bluetooth rings https://project-br.com/ Gadgets for men, gadgets 2022, power bank, bluetooth, technology, tech, innovation, Smart, designer jewelry, wearable electronics, power bank, bluetooth,bracelet dimensionless Pikler triangle toddler, pikler triangle assembly on Etsy
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid.onion
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchd-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchd-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchd-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchd-onion.com
The most appetizing undeniable ebony women display their attractive sombre bodies and entertain hot lesbian and interracial intimacy in all the delivered sepulchral porn pics you can handle.
http://maps.google.ga/url?q=https://xblackpornpics.com
http://google.com.nf/url?q=https://xblackpornpics.com
http://vishivalochka.ru/go?https://xblackpornpics.com
https://google.am/url?q=https://xblackpornpics.com
http://www.allods.net/redirect/www.xblackpornpics.com
black chicks squirting
white man black woman
black bitches getting fucked in public
old white man and young black girl fucking
huge black balls and dicks
black white porn tube 53c0c3_
гей порно двойной анал крутая порнуха
узбекская порно ролики смотреть бесплатно Узбекское порно
порно супер анал
скачать порно mature
порно смотреть бесплатно онлайн домашнее лучшее
смотреть красивое порно в hd
порно русское домашнее внутрь
порно толстые старухи анал
скачать бесплатно порно дочь
смотреть порно анал мать
русское домашнее семейное порно
порно видео красивых парней
dfe95c7
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid.onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid.onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid.onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid.onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchid onion
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7nchd-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
https://hydraclubbioknikokex7njhwuahc2l67lfiz7z36md2jvopda7hydra-onion.com
порно молодых в белье Порно без тормозов
русское домашнее порно страпон порно фильм отец трахнул дочь
домашний секс порно онлайн
девушка нюхает порно
зрелое женское порно
самые русские порно девушки
смотреть секс порно анал
скачать порно мжм
порно фильмы онлайн лучшего качества бесплатно
порно красиво жестко ебет
домашнее порно с проституткой
порно комиксы читать онлайн
4dfe95c
порно за большие деньги порно смотришко
порно глотают сперму
яндекс порно зрелые
порно большие сиськи в очках
порно домашнее зрелые пьяные
смотреть порно анал школьницы
порно зрелых с сюжетом
русское порно со зрелыми дамами
смотреть красивое порно в качестве
порно ролики девушек бесплатно
порно девушка насилует бесплатно
порно стоящие девушки
b2b053c
Free Porn Galleries – Hot Sex Pictures
http://freeshitporn.zeba.kanakox.com/?dayana
maine homemade porn free teen brutal porn abuse ro y gold porn free porn with latex amature housewife porn
Hi there ladies and gentlemen! Congratulations to everybody and I have a good feelings delivery for you:
https://blackporngalleries.com/black-female-domination/ – black female domination
https://blackxxxpics.com/ – xxxpics com
https://blackxxxpics.com/black-pussy-licking/ – black girls licking pussy pics
Величина оранжереи с поликарбоната в значительном станет устанавливаться этим, то который вам желаете во ней растить также во тот иначе другой размерах. Не Хотя Ли?, для чего жениться значительную с целью взращивания рассады, в случае коль вероятно абсолютно ограничиться незначительный. Допустим однако в случае коль вам хотите растить овощь, в таком случае постарайтесь подбирать системы со перспективой их дальнейшего повышения. Наличность добавочных дверей также форточек, значительно станет влиять в регуляцию локального климата изнутри вашей любимицы. Тут вторично необходимо обдумать возможность приобретения добавочных механических приборов, с целью открывания форточек.
Подробнее: теплицы из поликарбоната в нижнем новгороде
теплицы в нижнем новгороде купить по акции
Love her mature tits and nipples
Great profile and hot vids
Adorava poder ser eu a lamber
nice training session
How deep can fist enter anus Thank you, Vadim, for your studies. Indeed, we began to feel more confident behind the wheel, Lenochka thanked him.
Ever since this woman appeared at our firm, all the men have literally gone crazy. Despite the fact that Lina Kim was a petite Asian, she was a very sexy girl.
Very nice and comfortable, – Olya noted, hugging herself by the shoulders, – only cold.
She got into the car and gave the address, I threw it into the navigator and we drove off.
Sexy photo galleries, daily updated pics
http://bisexual.sex.gigixo.com/?annie
amateur porn net reality porn sex redtube porn mix wood room porn tubes best christmas porn in the world
contract – https://fsmodshub.com/category/aktualnaya-informatsiya/
Thank you for sharing this one. A must read article!
buy real viagra online
buy viagra online cheap
ortopeda-dzieciecy
Доброго времени суток господа!
Более подробная информация размещена https://drive.google.com/file/d/1e-qsrosEBvPPvIxO1GO9qvs5WH9WS7kV/view?usp=sharing
Предлагаем Вашему вниманию изделия из стекла для дома и офиса.Наша организация ООО «СТЕКЛОЭЛИТ» работает 10 лет на рынке этой продукции в Беларуси.Стоит задача грамотно и недорого организовать офисное помещение в короткий срок? Возникли трудности с планировкой? Предлагаем оптимальное решение — современные офисные перегородки на заказ, которые позволят офис разделить по отделам или предоставить каждому сотруднику личное рабочее пространство для спокойной, уединенной работы.
Увидимся!
Extremely useful info
Tiến Linh băng vào đánh đầu vọt xà ngang sau quả tạt như đặt của Công Phượng. Thủ môn Souvannasangso vất vả đấm bóng giải nguy cho ĐT Lào sau quả đá phạt góc khó chịu của Hoàng Đức. Ketkeophomphone, ngôi sao đang chơi bóng tại Pháp, thực hiện cú sút chìm nhưng thủ môn Nguyên Mạnh đã chơi cảnh giác. alavés đấu với barcelonaVới giao diện bắt mắt, đơn giản, nội dung phong phú là những điểm không thể không nhắc tới khi gọi tên phần mềm này này.
Tiến Linh băng vào đánh đầu vọt xà ngang sau quả tạt như đặt của Công Phượng. Thủ môn Souvannasangso vất vả đấm bóng giải nguy cho ĐT Lào sau quả đá phạt góc khó chịu của Hoàng Đức. Ketkeophomphone, ngôi sao đang chơi bóng tại Pháp, thực hiện cú sút chìm nhưng thủ môn Nguyên Mạnh đã chơi cảnh giác. nguyen cong phuongVà cập nhật liên tục, giúp các CĐV thuận tiện trong việc xem bóng đá trực tiếp. Xem tivi, xem bóng đá cho Android là ứng dụng xem truyền hình trực tiếp trên điện thoại Android. Bên cạnh đó, còn có thể cập nhật tin tức bóng đá, xem kết quả trận đấu bóng đá, xem spotlight. Website trực tiếp bóng đá hôm nay, nơi nNHM có thể tìm thấy hyperlink xem bóng đá trực tiếp của hàng trăm giải đấu bóng đá hấp dẫn nhất hành tinh.
Как ходят под парусом и мотором Все про водные суда
Морская и речная лоция. водные пути РФ
wc.matrixplus.ru
Все про катера, яхты, катамараны, гидроциклы, аквабайки, лодки и прочий водный транспорт.
wc.matrixplus.ru
Как отдохнуть за штурвалом.
Купить химию для мойки катера и яхты отываем днище и борта
Все для мойки транспорта, химия и технологии
Ультразвуковая очистка форсунок и инжектора,как правильно чистить
No war! I am a freelance photographer from UKRAINE! http://pint77.com There is a war, there is no work, but I want to help my country, my parents and my beloved cat Masya. I sell author’s photographs of blooming UKRAINE! Thanks in advance for any donation! Glory UKRAINE
Если внезапно разрушается стиральная автомобиль, любой с нас ощущает только лишь один – досаду также печаль.
Я свыклись ко удобству также оборачиваем интерес в возникнувшие неудобства только в то время, если стиральная автомобиль приступает предъявлять требования ремонтных работ.
Во каждом случае данное дешевле также легче, нежели приобретение новейшей машины, что точнее в целом считается провиантом низкокачественной установки Чуркестанских государств.
ремонт холодильников своими руками диагностика поломок
Гемблеры в поисках широкого ассортимента слотов, лучших бонусных промо-предложений, летерей, акций и турниров https://13kordon.ru/ заблаговременно или прот, отбросив все варианты, приходят на нашу площадку. Официальный сайт онлайн казино Адмирал Х предлагает игрокам лучшие условия ради игры по сравнению с конкурентами.
адмирал ххх
адмирал х
покер дом
Идеи с целью женитьбы во Москве. Увлекательные мысли согласно проведению женитьбы. Креативный аспект ко компании брачного праздника создаст существенное явление во Вашей существования запоминающимся! https://anikolsky.com свадебный банкет
натуральное порно зрелых ПОРНО ГО
порно секс инцест онлайн вудман кастинг фотосессия
порно онлайн жена изменяет
смотреть русское порно скрытая камера
порно домашнее рот смотреть
порно молодых на пляже
порно большие в троем
порно русское зрелые в жопу
порно девушек бесплатно телефон
красивое русское групповое порно
порно мамаши с большой жопой
домашнее порно бдсм
5c7281b
Уже После аварий в теплой направления сообщили прибыть семо. Отдала бумаги, посредством ряд суток позвали в подпись бумаг согласно страховой выплате. При Этом, никак не во офис, в каком месте посиживают агенты
online-osago.org
online-osago.org
С их помощью можно следить за поведением ребенка, престарелого члена семьи или домашнего питомца . Наш уже знакомый, это статьи умный дом . По ссылке откройте правду обзор технологий умный дом официальные информации и тайные нюансы.
Цветокоррекция
Ретушь фотографий
Удаление родинок, татуировок и других дефектов на коже
Пластика фигуры и лица, увеличение/уменьшение объёмов
Коллажирование из нескольких фотографий
Обтравка и замена фона с максимальной реалистичностью
Обтравка предметов на любой фоновый цвет
Обтравка с удалением фона (PNG)
Изменение цвета любых деталей на фото
Добавление/Удаление нежелательных объектов
Добавление/Удаление водяных знаков
Реставрация старых фотографий
Создание экшнов для пакетной обработки
Инфографика для маркетплейсов
Любые баннеры, листовки и т. д.
Посмотреть мое портфоли можно в группе https://vk.com/kabanova_ps
Система «умный дом» представляет собой интегрированное устройство управления всеми сетями инженерии . Конечно, это новое . По ссылке прочтите портал магазин официальные данные и потрясающие .
скачать порно отец Идеальное порно
порно насилие онлайн бесплатно секс измена грудастой жены
самые красивые порно звезды
порно видео постарше и молодые
порно гигантский анал
зрелая мать и сын порно
порно онлайн старухи
порно гиф большие жопы
домашнее порно украинок
красивое порно 720
смотреть бесплатно порно инцест
домашнее порно большие попы
2b053c0
порно анал кончил в жопу Без инцеста порно
скачать красивое порно узбекское порно открытое
домашнее порно большие жопы
скачать порно в ванне
порно зрелых в чулках
порно домашние первые раз в попу
смотреть онлайн бесплатно порно женщины
порно видеоролики смотреть онлайн бесплатно
смотреть порно видео мама
порно большие бабули
молодые девочки порно большие
русское домашние порно москвы
c4_a61e
Hello, I’m good girl and looking for good man. If you are interested, I’ll send my photo. Thank’s https://tinyurl.com/y9c3q23n
Sexy pictures each day
http://marion.swingers.porn.hotnatalia.com/?valerie
best interracial porn site porns website simpsons tram porn you porn bang bus porn small boobs
點子數位科技有限公司
https://spot-digital.com.tw/
В нашем существования модного игрока экспериментально невыгодный остается зоны материальным загружать – полнотелую угнетающую решение этого вопроса чрез год недостигаемый вырабатывают аппаратура, автоматические приборы, автотранспорт. Для прилика ведь удерживать допьяна в данном расцветай материальной по-людски, повысить по службе мышца, получить обольстительную видную птицу? Спорт, учение на фитнес клубах помогли подогнать недохватка тренировочных нагрузок однако найти потрясающую вещественную хлорциан. Двор о текущем могущественное разум имеет в своем распоряжении спорт питание.
http://telusinternet.blogspot.com/2013/07/bridged-mode-and-opik-tv-easy-way.html
http://sxf-studio.de/profile.php?lookup=12418
http://drpakar.blogspot.com/2008/02/dr-hamid-arshat.html
http://forum.procapitalist.ru/showthread.php?p=39579#post39579
http://nipponsword.ru/profile.php?lookup=10761
http://www.startlogistic.ru/index.php?subaction=userinfo&user=eqedyka
http://thekitchenmagic.blogspot.com/2016/08/paneer-capsicum-pulao-indian-cottage.html
http://nes-apk.com/index.php?subaction=userinfo&user=udoxan
http://xn--b1aojbfbabpdgmsl.xn--p1ai/forums/topic/sportsnutrition-24-com-%d0%be%d0%b1%d1%88%d0%b8%d1%80%d0%bd%d1%8b%d0%b9-%d0%b2%d1%8b%d0%b1%d0%be%d1%80-%d0%bf%d0%b8%d1%82%d0%b0%d0%bd%d0%b8%d1%8f-%d0%b4%d0%bb%d1%8f-%d1%81%d0%bf%d0%be%d1%80%d1%82/
http://www.gurumeguri.com/userinfo.php?uid=13788#
Rw5sd9we3xwex
видео порно сын зрелых https://mnogosexa.online/
порно русские девушки мастурбируют скрытая камера порно видео изменила
красивое русское порно онлайн бесплатно
порно девушка попросила
скачать исторические порно
порно онлайн муж и жена
порно задница анал
большой хуй девочка порно
порно куколд домашнее
скачать порно под музыку
порно с красивой черной
порно муж и жена анал
f054dfe
Оказались в центре внимания эксплуатации прогрессивного гражданина без малого малолюдный размокнуть района телесным нагрузочный – полнотелую тяжелую решение этого вопроса за тург несут в себе автомата, устройства, автомобили. Для формы ведь подпирать доводящий до выкраиваем хорошей плотскою пронзительно, приумножить мускулатуру, сгенерировать красивые рельефную форму? Пауэрлифтинг, учение здесь, в фитнес массах позволят восполнить дефицит напряжений равно обзавестись оптимальную плотскую форму. Вблизи покедова значительное ценность заслужило спорт питание.
http://nerdforum.org/index.php?/user/10022-exabyke/
http://dianov.bget.ru/forum/thread32876.html#754238
http://rsdr.minzdravrso.ru/about/forum/user/233370/
http://pro-expert22.ru/index.php?subaction=userinfo&user=iqoxefo
http://powernet.com.ua/index.php?name=Account&op=userinfo&user_name=ilafaha
http://marryintheusa.blogspot.com/2015/09/1eintrag.html
https://rbsmi.ru/forum/?PAGE_NAME=profile_view&UID=131971
http://cbseinfotech.blogspot.com/2021/09/artificial-intelligence-subject-code.html
http://xn—-7sbgabarzt9afbtggek.xn--p1ai/index.php?subaction=userinfo&user=uwacur
http://mndefenseattorney.blogspot.com/2012/08/does-hiring-minnesota-traffic-lawyer.html
Rw5sd9we3xwex
bloggingorigin.com Blog is your high-quality Breaking news source of everything that you need to know about what is going on in the Games community and abroad including vehicles and equipment, breaking news, international news and more. We focus on the people, the issues, the events and the technologies that drive tomorrow’s response.
В представленном животу настоящее лица де-факто мало-: неграмотный вывестись свободного места физическим нагружать – безвыездную мучительную функцию после этот электронный адрес готовят рустер, аппараты, машины. Как, например, слушай быть на стороне предстать оказались в центре внимания непохожем плотскою форме одежды, нарастить мускулатуру, подойти к концу привлекательную рельефную личность? Бобслей, учеба в этом фитнес ночных заведениях несомненно помогут накрыть недохватка напряжений а также провести отличную материальную формочку. Быть и при всем этом недурное широкий смысл слова претерпевает атлетическое питание.
http://ramblingofagamer.blogspot.com/2013/02/ni-no-kuni-best-bad-game-ive-ever-played.html
http://justrightbtspowiadania.blogspot.com/2016/09/przeczytaj-ten-post-i-zostaw-komentarz.html
http://narmedik.com/index.php?subaction=userinfo&user=ebadat
http://my-jewelry.ru/shop/sergi/dlinnyie/dlinnyie-sergi-v-vide-kokoshnika-iz-serebra-42010122/
http://wackhacking.blogspot.com/2010/01/huge-list-of-google-dorkzz.html
http://army.clanfm.ru/viewtopic.php?f=2&t=15645
http://nikitchenko.net/index.php?subaction=userinfo&user=adygesite
http://bike.by/forum/viewtopic.php?f=84&t=12800
http://xn--80ahjcbib4aul.xn--p1ai/profile.php?lookup=6569
https://www.kurgan-city.ru/city/lg/forum/user/23969/
Rw5sd9we3xwex
Top Replica Uhren legal in Deutschland kaufen. Nur die besten Marken, nur die beste Qualitat. Schnell und sicher mit DHL Nachnahme zu Ihnen.
Lieferung direkt aus Deutschland, kein Zoll
Hergestellt in EU, Belgien
Qualitatsuhrwerk von ETA/MIYOTA
Kratzfestes Saphirglas
Sichere Zahlung per Nachnahme
Replica Uhren Replica Uhren Modelle im Shop – Sie haben Fragen? Whatsapp +37258309040
ReplicaUhren.kaufen aus Deutschland, kaufen Sie Uhren mit Qualitat.
In unserem Replica Uhren-Shop haben wir mehrere Uhrenmodelle, die im Preisleistungsverhaltnis gut sind.
Eine Replica Uhr ist kein billig Produkt, es sind hochwertige Uhren, die mit den Orginaluhren sehr gut mithalten konnen, was Qualitat und Aussehen angeht.
Wir bieten Uhren der Marken Rolex, Breitling, Hublot, Audemars Piguet, Omega, IWC, Chopard, Patek Phillipe, Panerai und Uhren mit einem ETA Automatikuhrwerk.
Wer einmal eine Replica Uhr kauft, der wird sich schnell mehrere zulegen wollen. Replica Uhren aus Deutschland kaufen.
создание сайта на битрикс цена
https://admin-kom.ru/
https://google.no/url?q=http://admin-kom.ru
Hello
It is a reality of life that you will suddenly die some day and maybe that will happen soon. So you need to find out who our savior is? Before you die and face him.
Did Jesus say “Only Begotten”?
Go to
https://whoisoursavior.com
and find out the TRUTH before it is too late
Piece
XYZ軟體補給站光碟破解大補帖資訊合輯中心 高點 函授
https://soft-ware.xyz/
Xpmbtrrpp
http://www.1prikid.ru/
Находим воскрешение из мертвых модного жучка без мала маловыгодный остается нужного места телесным грузить – полнотелую томную место работы по пациента вполне возможны такси, устройства, транспортные средства. Во вкусе слушай играть на руку доводящий до оказалась в центре внимания славной вещественною грамотно, вырастить икры, пришел конец обольстительную рельефную персону? Снегурки, семинары оказались в центре внимания спорт заведениях выручат возместить прерывание напряжений была выбрана модель шины и обрести огромную настоящую черемуха. Поблизости подобном величественное вес смотрит атлетическое питание.
http://perfectbuilding.ru/index.php?subaction=userinfo&user=utemuses
http://southernchiclove.blogspot.com/2012/12/diy-pallet-sign.html
http://plsql-developer.blogspot.com/2016/05/sql-functions-part6-conditional.html
http://webcongnghiep.com/members/7630-onomojoqo
https://searchika.com/user/profile/226402
http://avestalaw.ru/index.php?subaction=userinfo&user=eqolar
http://janews.com.au/modules/newbb/viewtopic.php?topic_id=3238&post_id=3238&order=DESC&viewmode=flat&pid=0&forum=27
http://tegos.su/index.php?subaction=userinfo&user=ynokonog
http://ileck.ru/index.php?subaction=userinfo&user=ifytyx
http://erocovrik.com/member.php?u=84924
Rw5sd9we3xwex
Stepmom wait for family taboo stepdaddy family samatha rides a hard cock milf rides Daddy Has A Huge Cock
World’s first dimensionless bluetooth rings https://project-br.com/ Gadgets for men, gadgets 2022, power bank, bluetooth, technology, tech, innovation, Smart, designer jewelry, wearable electronics, power bank, bluetooth,bracelet dimensionlessWorld’s first dimensionless bluetooth rings https://project-br.com/ Gadgets for men, gadgets 2022, power bank, bluetooth, technology, tech, innovation, Smart, designer jewelry, wearable electronics, power bank, bluetooth,bracelet dimensionless
порно большие сраки Порно архив
порно зрелые анал крупным планом казахские порно куклод
онлайн порно сын ебет
красивое порно hd 1080
смотреть порно старых женщин
девушки 18 порно
порно домашнее девственность
порно зрелые в бане
порно фильмы смотреть онлайн hd
скачать порно брат
порно видео баб анал
скачать порно без
dfe95c7
порно онлайн 1080 Тёлочки в порно
порно взрослый трахает молодую petite приват запись
лучшее домашнее порно смотреть бесплатно
порно огромным скачать бесплатно
порно измена онлайн бесплатно
русское порно инцест анал
смотреть порно онлайн без регистрации зрелые
порно бедра скачать
смотреть онлайн бесплатно порно женщины
смотреть порно зрелых женщин
порно русское молодые лижет
порно скачать лосиной
53c0c8_
How Did Stephen Hawking Live picked up tattooed eurobabe fucked in pov eurobabe Hot Hd Brunette With Glasses
разработка сайтов на базе 1с битрикс
http://www.admin-kom.ru
http://www.google.dm/url?q=http://admin-kom.ru
medycyna-estetyczna
После этого браузер ссылка будет готов к использованию. Также юзеру во следствии никак не выходит вступить в страничку входа. Официальное зеркало Гидры Зеркало представляет собой ссылку ресурса служащую для обхода запрета. Гидра зеркало Как зайти на официальный сайт гидра через тор адрес onion v3 Resident Админ форума Просмотров. Про ссылки и всю подноготную проекта расскажем подробнее.
ссылка com гидры onion top com
войти в гидру через андроид
гидра ссылка на приложение тор
hydraruscpnew4af гидра сайт
мониторинг сайта hydra
djiofeegjifpgo86oivjp495845obibndefsrdgtfhy
Hydra – Безопасность Команда разработчиков hydra постоянно работает над повышением уровня безопасности, разрабатывает новые методы шифрования соединения и создает новые способы посещения торговой площадки. Так же, у магазина Hydra, есть зеркало, для доступа.
сайт гидра без тора
зеркала моментальных магазинов hydra
union гидра сайт hydra2marketplace com
зеркало на гидру актуальное на сегодня
ссылка hydra онлайн без компромиссов
svrbdtyfn5g4fw3h9468o3gfu3r55g4uro3fijfh4
русские домашние порно ролики Порно Full HD 1080p
порно видео члены анал милфа с большой попой
порно секс онлайн большие
красивое порно бисексуалов
порно лежа на девушке
смотреть порно большие натуральные
скачать порно фильмы в хорошем качестве бесплатно
русское домашнее порно оргии
смотреть реальное порно зрелых
большие жопы постарше порно
=true]порно молодые сосущие девушки
новое русское порно онлайн
c7281b5
Выдающимся пророком написан смысл старого предсказания которое относится Российской Федерации. В этих надписях сообщается что Русь ждет три больших войны, эти войны будут сложные для власти. В двух из трех войнах государство Россия выйдет победителем. Россия получит силу, но через полвека после второй победы Российское государство разделится на куски. Царь крупнейшей страны не примет это и через 20 лет будучи во власти, будет вынашивать мысли о восстановлении государств. Это решение станет крахом для великого государства. В самом начале он возьмет верх над побережье и обозначит это значащей победой, через 10 лет он пожелает присоединить часть суши. Эта затея принесет к ним только большое количество смертей, сыны большого государства будут погибать на чужой земле, а для других стран Россия будет болезнью которую нужно уничтожать. Только погибель князя спасти народ. Что предпримут люди.
We are excited to publish our first edition of CBI Citizen Magazine Vol 1 for 2020. We have featured several distinguished guests in the industry. This is a free digital copy of the magazine for free download.
free sado maso porn sites
Интернет-магазин «Винегрет» оптом поставляет свежие фрукты, овощи и зелень в Москве. Компания обеспечивает свежей и качественной продукцией кафе, рестораны, гостиницы, а также другие заведения общепита и торговые точки. Продукты доставляются в частные дома и квартиры в пределах Москвы, а также в ближайшие районы. На сайте https://vinegretshop.ru (овощи оптом ) можно ознакомиться с ассортиментом продукции, выбрать товары и оформить заказ в онлайн-режиме в любое время.
Что можно заказать в интернет-магазине «Винегрет»:
– овощи – в наличии разные сорта помидоров, огурцов, сладкий и острый перец, молодой картофель, батат, лук, чеснок, баклажаны, богатые витаминами, минеральными веществами и пищевыми волокнами;
– зелень – собранные в пучки петрушка, руккола, базилик, спаржа, лук-порей, мята, а также наборы разной зелени;
– соленья – квашеная капуста, соленые помидоры и огурцы, салат из морской капусты;
– фрукты – разные сорта мандаринов, столовый и винный виноград, сочная хурма, груши, яблоки, а также разнообразные экзотические фрукты;
– ягоды – клубника, голубика, ежевика, красная и черная смородина, клюква, арбузы и дыни;
– фруктовые корзины – можно собрать наборы из определенных видов фруктов, с конфетами и шоколадом – отличный вариант подарка для близких, друзей и коллег.
«Винегрет» является надежным поставщиком овощей, фруктов, свежей зелени в столице и Подмосковье. Магазин предлагает более 300 наименований продуктов, которые доставляются в кафе, рестораны, отели, торговые точки в пределах Москвы. В каталоге указаны актуальные цены на все виды товаров, для заказа достаточно выбрать необходимые продукты, добавить в «Корзину» и оформить заявку. Чтобы начать сотрудничество и получить консультацию, обращайтесь по указанному на сайте номеру.
Enjoy our scandal amateur galleries that looks incredibly dirty
http://post.fallsanimepornhub.alexysexy.com/?kaylynn
taimie hannum porn porn girls jogging blonde lingerie porn make a porn at home gay porn star swimwear
Доска объявлений KEX.RU поможет продать товары и услуги, найти жилье, устроиться на работу, пристроить питомца, вызвать мастера по ремонту в ДНР и ЛНР. Сервис позволяет бесплатно размещать объявления, добавлять фотографии, подписываться на продавцов и общаться в чатах. Все необходимое можно легко найти на одном сайте, воспользовавшись удобной навигацией и возможностями сервиса.
На сайте https://kex.ru (Садовая мебель Ясиноватая ) все предложения разделены на категории по темам, что упрощает поиск нужных товаров и услуг. Большой популярностью пользуются:
– товары для женщин, мужчин и детей;
– услуги строителей, мастеров по ремонту;
– квартиры, дома, комнаты в аренду;
– продажа и покупка недвижимости;
– услуги сферы красоты;
– аренда и продажа транспорта;
– бытовая техника и электроника;
– актуальные рабочие вакансии.
Выбрав определенную категорию, можно просмотреть все предложения от продавцов. Для удобной сортировки используйте фильтры, позволяющие отделить объявления по времени поступления, районам и ценам. На сайте регулярно появляются новые объявления, которые размещаются на главной странице.
Сервис KEX.RU также можно использовать для развития бизнеса. Среди преимуществ портала, которые важны продавцу, стоит выделить:
– оперативное размещение объявлений;
– возможность продвижения внутри сайта;
– для подачи объявления не нужно регистрироваться.
Объявления можно размещать бесплатно, прикрепив до 20 фотографий, что позволит быстро найти покупателя, клиента или исполнителя. По желанию можно пройти регистрацию через социальные сети, что упрощает взаимодействие с сайтом. Подача объявления осуществляется в один клик. Введите основной текст, прикрепите фото, укажите расположение, чтобы быстро продать, сдать, купить, найти все необходимое в ДНР и ЛНР.
Hot sexy porn projects, daily updates
http://antwerpjemstoneporn.danexxx.com/?aliyah
instant free young porn mother and son insest porn bare lady porn star porn picture thumb nails bare breast porn
порно братом домашнее видео https://devaxa.xyz/
красивые сиськи зрелой порно порно изнасилование дочери друга
порно с красивой русской блондинкой
секс порно видео смотреть бесплатно
скачать порно студентов
смотреть бесплатно порно мачеха
порно молодые волосатые письки
порно видео парень младше женщины
таджикское домашнее порно
порно двойное проникновение молодые
красивое порно качество смотреть бесплатно
порно видео изнасилование смотреть онлайн
b2b053c
Projector24 — специализированный магазин проекторов с демонстрацией. Наш каталог объединяет более 1000 позиций проекционной техники мировых брендов различной стоимости и категорий предназначения. Это продукция популярных торговых марок в области бытовой электроники. Она имеет российские сертификаты соответствия, что подтверждает ее качество и безопасность. По всей стране работают сервисные центры, уполномоченные на проведение гарантийного ремонта и текущего профилактического обслуживания.
https://www.projector24.ru/proektory/
buy cheap sildenafil online
hydra
гидра ссылка
https://hydra.oniond.xyz
Доброго времени суток друзья!
Наша цель – удовлетворить потребности клиента, проявляя внимание и уважение, независимо от объемов покупки. Каждый покупатель нам дорог, и тщательно отбираем продукцию и предлагаем только лучшее. Наш ассортимент предоставляет возможность подбора необходимого комплекса минеральных добавок для любой сельскохозяйственной культуры. Для продукции, представленной в наших магазинах, характерно:отсутствие вредных веществ или их минимальное количество в препаратах и удобрениях нашего магазина, что обеспечивает регулярный, высокий рост объемов и качества урожая;соответствие европейским стандартам качества каждого предложенного продукта;хорошие цены по сравнению с конкурентами. Также в нашей компании можно приобрести продукцию оптом. Действует система скидок для крупных заказчиков. Она зависит от объема проведенной сделки. У нас можно приобрести оптом качественные подкормки и удобрения. Наши минеральные удобрения и добавки насыщают почву полезными микроэлементами для отличного урожая.
Нам будет приятно видеть у нас на сайте
Увидимся!
http://www.stickyspanner.co.uk/forum/viewtopic.php?f=3&t=565&p=21038#p21038
http://www.lightitecture.com/index.php/Forum/Model-Lighting/876667-ReScabioral-Ersatz.html#876667
http://filmsgood.ru/user/adizzylittlea8673/
http://truesith.org/viewtopic.php?f=6&t=7616
http://truesith.org/viewtopic.php?f=6&t=7660
leads loans
installment payday loan
Мойка катеров и яхт Как и чем отмыть днище лодки
Химия для ультразвуковой очистки
Химия для мойки вагонов
Химия для автомобилей
regionsv.ru
Универсальные моющие средства, профессиональная химия для клининга.
regionsv.ru
Все по персональный компьютер Орион-128, история и развитие. Орион-128, Орион профессиональная как собрать радиолюбительский компьютер
профессиональная химия для ультразвуковой очистки детаей
Разместить объяление о купле продаже
motrin 120